Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
Reconstruction of the facial skeleton
Effective reduction and fixation of the facial skeleton can be carried out at any time within the first 2 weeks of injury. There may indeed be considerable advantages in delaying treatment of comminuted mid-face fractures, which are more difficult both to assess and reduce in the presence of the considerable facial oedema which is often an early feature. There are a few fracture patterns which demand early reduction even if fixation has to be compromised in the short term. These are: 1.Mobile, painful, nearly always multiple, mandibular fractures which interfere with swallowing and increase restlessness in a patient with a significant head injury. 2. Facial fractures associated with continuing haemorrhage into the airway. 3. Upper mid-face fractures accompanied by profuse cerebrospinal fluid leakage. 4. Impaction of the mandibular condyle into the middle cranial fossa. 5. Dento-alveolar fractures with subluxed or fractured teeth. The principles which determine the sequence of reduction and fixation of multiple fractures of the facial skeleton are based on the surgical anatomy. The mid-face is represented by a complex of bones which have to be contained in their correct positions within that outer frame, and finally the projecting nasal complex must be reassembled on a firm foundation. The techniques of reduction and fixation of the individual components of the face will be described in later chapters, but the sequence of reduction and fixation needs to be understood from the outset. Transfixation with Kirschner wires Kirschner wires (K-wires) are widely used in orthopaedic practice and are therefore usually available in most hospitals. In rare emergency situations these wires can be used to provide temporary stabilization of a fractured mandible. The fracture is held in a reduced position and one or more wires drilled through the fragments so that part of the wire passes through undamaged bone each side of the fracture. The method is versatile and can be applied with appropriate ingenuity to fractures in any part of the mandible whether there be teeth present or not (Vero, 1968). In the context of fractures of the tooth-bearing area it is of little use when more conventional methods are available. Shuker (1985) described an ingenious use of a single K-wire for the rapid immobilization of a comminuted fracture of the body of the mandible such as might occur after a missile injury. A horseshoe-shaped 2 mm K-wire is adapted to the mandibular arch and then each end is inserted into two holes drilled from an intra-oral approach into the anterior border of each ramus. The horseshoe-shaped wire lies on the buccal side of the displaced mandibular arch and the individual segments with their contained teeth are ligatured to this semi-rigid frame. Methods of immobilization The fact that there is no uniformly accepted method of immobilizing edentulous fractures is indicative of the fact that no completely satisfactory method has yet been devised. There is no doubt, however, that the traditional treatment by means of Gunning-type splints has been largely superseded in recent years by methods which employ some form of direct or indirect skeletal fixation. In older patients intermaxillary fixation is even less desirable than in younger age groups. Nutritional requirements become difficult to maintain and oral candidiasis commonly affects the oral mucosa causing considerable discomfort during the active treatment period. The methods of treatment currently available are listed below: 1. Direct osteosynthesis: (a) bone plates; (b) transosseous wiring; (c) circumferential wiring or straps; (d) transfixation with Kirschner wires; (e) fixation using cortico-cancellous bone graft. 2. Indirect skeletal fixation: (a) pin fixation; (b) bone clamps. 3. Intermaxillary fixation using Gunning-type splints: (a) used alone; (b) combined with other methods. Direct osteosynthesis Bone plates are particularly useful for displaced fractures of the edentulous mandible, particularly those at the angle. They allow the fracture to be stabilized without immobilization of the jaw as a whole. The patient is, as a result, more comfortable during the period of healing of the fracture. The main mandibular plating systems described earlier in the chapter are in general applicable to edentulous fractures. Unlike the dentate mandible there is a significant risk of non-union in the edentulous state and it could be argued that compression plates might have a theoretical advantage. However, the reduced depth of bone in the edentulous mandible favours the use of non-compression miniplates rather than the bulkier compression plates in that the former are less likely to interfere with the edge of a future denture. Bone plates are easier to apply in the edentulous state than when teeth are present as there is no need to achieve the same degree of precision in the reduction of the fracture. Any discrepancy in the eventual occlusion of the pre-existing dentures is more easily corrected than when natural teeth are involved (Fig. 10).
It is easier to apply bone plates to the edentulous mandible than it is to insert transosseous wires. There must be fairly liberal exposure of the fracture site with extensive elevation of the periosteum, but that exposure can be confined to one surface of the bone and the overall peri-osteal attachment is often disturbed less than when inserting a number of transosseous wires. Both compression and non-compression systems require an adequate blood supply to achieve uncomplicated bony union and elevation of periosteum in the thinner mandible seriously compromises the blood supply to the fracture site. It has been suggested that in these circumstances plates should be applied with an intervening layer of attached periosteum, but in practice this is difficult to accomplish. Plates related to the denture-bearing part of the mandible are much more likely to require removal at a later date than those used in the ramus or in dentate fracture sites. Nevertheless some form of plating is currently the preferred method of fixation for the majority of edentulous mandibular body fractures. Resorbable plates would appear to have an advantage but, at their present stage of development, degradation takes place over a period of 2 years or more during which new dentures are likely to be needed. A metal plate removed electively is a better option.
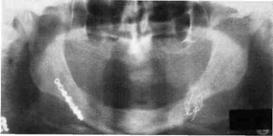
Figure 10. (a) Panoral tomogram of a bilateral fracture of an edentulous mandible with considerable displacement of the fragments, (b) The situation 6 months after treatment. A miniplate was used for fixation on the right and transosseous wiring on the left. No IMF was employed and the healing on each side is comparable. 6. MATERIALS FOR SELF-CONTROL: A. Questions for self-checking: 1. X-ray foto, a photo and discharge from a hospital from histories of the victims with bones fractures. 2. Materials and the equipment for preparation for operative treatment of fractures of jaws. B. Tasks for self-checking: 1. To the victim with a fracture of the maxilla by Le Fort ІІ type operative intervention with fastening fragments by spokes by kirshner entered through a skin in a cross-section direction at a level of zygomatic bones is carried out. Name a method of an osteosynthesis by authors. (The answer: by Makienko). 2. At the fighter who is injured with a debris of shell, is diagnosed a ballistic fracture of the mandible with defect of a bone in the chin region more than 3 sem. What method of fixing of fragments of the mandible is shown? (The answer: the osteosynthesis by Rudko and by Bernadsky with apparatus method).3. Patient of 42 years is hospitalized with fracture of the maxilla on type II by Le Fort. Choose the device for treatment of this patient. (The answer: by Zbarsh).
C. Materials for the test control. Test tasks with single right answer (α = ІІ): 1. Name the indication for application of device by Zbarzh. A. Fracture of the maxilla by Le Fort I, ІІ, III, by Geren, by Vasmund. B. Fracture of the mandible at absence of the teeth on jaws or at defect of a body of a jaw. C. Fracture of the branch of mandible or process condilaris. D. Fracture of the mandible within the limits of a dental lines or the angle of the mandible.E. Fracture of an alveolar or coronal process of the mandible. (Correct answer: А.). 2. What kinds of fixing concern to a direct type of osteosynthesis at fractures of the maxilla? A. Imposition of spokes by Kirshner, spokes by Makienko. B. Imposition of pin devices. C. Imposition of circular ligature. D. Impositionof a bone seam and a metal frameworks. E. Imposition of wire, banded tape or cast arch bar. (Correct answer: А). D. Educational task of 3-rd level (atypical tasks): 1. Patient С., 28 years, has addressed in 3 days after a trauma. Complaints to a painful swelling in a site of a body of the mandible at the left. Palpation of the body of the mandible at the left side is painful, it is marked mobile оf fragments in a site of 45 teeth. On the X-ray in lateral left projections the crackor fracture line in a site of 45 teeth. The diagnosis is exposed: a fracture of a body of the mandible at the left in a site of 45 teeth. What kinds of surgical treatment should be applied? (The answer: not a direct osteosynthesis). 2.Patient С., 58 years, has addressed in 5 days after a trauma with complaints to a painful swelling in a site of a body of the mandible on the right. Palpation of the body of the mandible at the left side is painful, it is marked mobile of fragments in a site of 35 teeth. On the X-ray in the left lateral projections revealed crack of the bone in the site near the roots of 35 teeth. The diagnosis is exposed: fracture of the body of the mandible on the right side near roots of 35 teeth. What complication is authentic in the given clinical case? (The answer: a suppuration of a bone wound). 3. The patient T. 75 years, has arrived in hospital with the diagnosis: fracture of the angular region of mandible on the right side with displacement. Objectively: asymmetry of the face due to a posttraumatic edema, at palpation is marked mobile of fragments in a site of the fracture, a pain. In the anamnesis - epilepsy since a birth. What method of treatment do you offer? (The answer: the osteosynthesis).
Theme № 17 Combine damages of maxillofacial area. Cranial - maxillofacial damages. Features of clinical current, diagnostics, complications, features of treatment at stages of medical evacuation. Achievement of native scientists, members of chair. 1. ACTUALITY OF THEME. Knowledge of a clinical picture, features of diagnostics of combine damages of maxillofacial area and their complications, methods of treatment which will allow the doctor - stomatologist to render medical aid by the maxillofacial wounded in a wartime and in conditions of extreme situations. 2. СONCRETE AIMS: 2.1. To analyze a concept about combine damages of maxillofacial area. 2.2. To explain the mechanism of a symptom of mutual burdening. 2.3. To offer the etiological and pathogenetic scheme of a symptom of mutual burdening. 2.4. To classify cranial - maxillofacial damages and a brain traumas. 2.5. To treat the data of X-ray pictures, tomograms and other results of victims with a combine trauma in maxillofacial surgery. 2.6. To draw schemas of stages of medical evacuation. 2.7. To analyze possible complications of combine traumas in maxillofacial region. 2.8. To make algorithm of first aid, examination and treatment at stages of medical evacuation of victims with cranial - maxillofacial damages and a traumatic illness.
|
||||||||||
|
Последнее изменение этой страницы: 2021-01-08; просмотров: 54; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 3.12.71.237 (0.01 с.) |