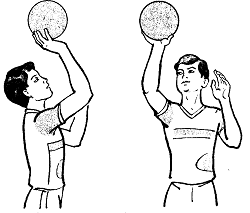
Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
SARS-Cov-2 эволюционирует по крайней мере в течение 7 летСтр 1 из 7Следующая ⇒
Лот 1 SARS-Cov-2 эволюционирует по крайней мере в течение 7 лет Д-р Лиджи Томас, доктор медицины
Нынешняя пандемия COVID-19 демонстрирует огромную неизвестность вирусологии, которая по-прежнему бросает вызов способности человечества оставаться здоровым перед лицом патогенов. В то время как большинство известных микробов имеют ограниченную близость к конкретному виду, продолжая адаптироваться к организму хозяина, коронавирус 2 с острым респираторным синдромом (SARS-Cov-2) перешел от неизвестного животного резервуара, как предыдущие SARS и MERS коронавирусы, чтобы заразить человеческие клетки. Такие вирусы, как правило, легче инфицируют и вызывают более серьезные заболевания, поскольку они еще не полностью адаптировались к целевому хозяину. Жгучий вопрос заключается в том, каким образом новые вирусы приобретают способность распознавать, связываться с клетками человека и проникать в них впервые - зависит ли это только от вирусных белков, распознающих белки клеток-хозяев, или адаптации в других вирусных процессах, которые позволяют репликацию в организме человека. Этот вопрос обсуждается исследователями Калгарийского университета в новом исследовании, опубликованном на сервере bioRxiv* в июне 2020 года. Шипованный белок является наиболее известным из белков SARS-Cov-2, и его связывание с рецепторами ACE2 на клетке-хозяине отвечает за проникновение вируса в клетку-мишень. Человеческий ACE2 (hACE2) имеет несколько редких вариантов, которые делают хозяина более уязвимым к инфекции. Аналогичным образом, белок шипа этого вируса имеет большую аффинность к рецептору, чем предыдущий SARS-вирус, что является другим возможным объяснением повышенного инфекционного потенциала текущего вируса. Последствия заключаются в том, что, во-первых, аффинность шипа-РБД к hACE2 не является основным фактором, определяющим высокую инфекционную природу нынешнего вируса, поскольку этот вирус предков был способен сделать то же самое. Во-вторых, исследователи предполагают, что этот вирус даже тогда был способен плотно связываться с рецептором. Поэтому этого недостаточно для получения наблюдаемой в настоящее время способности к быстрому и широкому распространению среди людей. Вместо этого, это должно быть связано с другим набором мутаций в вирусном геноме.
Ещё одним последствием является то, что нынешний вирус, возможно, вообще не перешел на людей животного происхождения, потому что его близость к hACE2 не была недавно приобретённой молекулярной особенностью. Это может означать, что способность заражать человеческие клетки существовала в течение более продолжительного периода времени в прошлом, но вызывала менее очевидные или меньшие клинические симптомы, которые прошли незамеченными. Другая альтернатива заключается в том, что она затрагивает лишь небольшое число людей, позволяя ей оставаться в поле зрения общественного здравоохранения.
Срок полномочий - 2 Срок З Аллергии и генетика Аллергические заболевания очень распространены в современном обществе, и до половины всех детей в Великобритании были диагностированы по крайней мере с одной астмой, атопической экземой, сенной лихорадкой или пищевой аллергией. В связи с этим ростом заболеваемости аллергией возникает вопрос о развитии этих заболеваний в целях содействия профилактике и лечению. Аллергические условия Существует несколько аллергических состояний, которые часто сгруппированы при обсуждении связи между аллергией и генетикой, включая астму, атопическую экзему, сенную лихорадку или пищевую аллергию. Эти условия, как представляется, связаны между собой и имеют схожую структуру в отношении генетической восприимчивости. Дети, страдающие аллергией, часто следуют схеме, где они пройдут через ряд аллергических состояний, известных как аллергический марш. Например, они могут сначала испытать атопическую экзему с последующим спадом, за которым следует появление астмы, а затем ринита. У некоторых детей также возникнут некоторые аллергические заболевания и они сохранятся на всю жизнь Родственная связь Некоторые семьи, как представляется, в большей степени подвержены аллергическим заболеваниям, чем другие, и дети, родившиеся в этих семьях, подвержены более высокому риску развития аллергического заболевания. Считается, что эта семейная тенденция к развитию аллергических состояний имеет генетическую связь, известную как атопическая.
По оценкам, у более чем половины детей, родившихся в атопических семьях, может развиться аллергическое заболевание, в то время как заболеваемость детей, не имеющих в семье аллергического заболевания, составляет один из пяти. Этот риск еще более возрастает в семьях, в которых оба родителя страдают аллергией. Примечательно, что у детей не всегда развивается та же аллергическая болезнь, что и у других членов семьи, и исследования, как правило, указывают на восприимчивость к аллергии, а не к конкретному аллергическому заболеванию. Генетические исследования Исследования ассоциации генома (GWAS) помогли нам лучше понять гены в развитии аллергических состояний. Специфические генные вариации, которые изменяют кодирование цитокинов, полученных эпителиальными клетками, таких как интерлейкин-ЗЗ и тимический стромальный лимфобиетин, могут быть вовлечены в патогенез аллергии. Кроме того, вариации генов ORMDL3 и GSDML были связаны с повышенным риском ранней астмы. Эти находки помогают идентифицировать детей с наиболее высокой восприимчивостью к аллергии, что может быть полезно при выборе профилактических методов или осознании симптомов аллергии, требующих лечения. Тем не менее, в области исследований аллергии и генетики предстоит еще много сделать. Необходимы дальнейшие исследования для дальнейшего углубления понимания механизмов генетического развития аллергических состояний и начала применения методов, направленных на уменьшение воздействия аллергии на современное население. БИЛЕТ 4 1. High Blood Pressure in Children. By Sally Robertson, B.Sc.
Although people usually assume that only middle-aged or elderly people develop high blood pressure (hypertension), it is also possible for the condition to arise in teenagers, children and even babies. The American Heart Association advises that all children should be checked for high blood pressure on a yearly basis, as detecting the condition and treating it early will improve the child’s health and reduce or prevent the harmful effects of the condition. Causes Hypertension in children is usually caused by another underlying health condition such as heart disease or kidney disease. Itis therefore referred to as secondary hypertension and once the medical condition is resolved, the blood pressure typically returns to normal. Secondary hypertension may also be caused by the following conditions: Hyperthyroidism Adrenal disorder Sleep problems, particularly sleep apnea Renal artery stenosis Some medications can increase blood pressure, but, again, the blood pressure usually returns to normal if the medication is discontinued. In some cases, a doctor cannot determine what is causing the hypertension, in which case the condition is referred to as primary or essential hypertension. Various factors that are known to contribute to the risk of primary hypertension include: Overweight or obesity (body mass index >25) Family history of hypertension High cholesterol and triglycerides Type 2 diabetes or raised fasting blood sugar Complications Children with hypertension often develop sleep apnea and breathe abnormally while they sleep, particularly if the child is overweight. If the hypertension persists into adulthood, the person is at an increased risk of kidney disease, stroke, heart attack and heart failure. Tests and diagnosis Blood pressure is measured using an inflatable arm cuff and blood pressure gauge. The blood pressure measurement is made up of two readings. The first (upper) number is a measurement of systolic blood pressure, which is the pressure in the arteries when the heart beats. The second (lower) number is a measurement of the diastolic pressure, which is the pressure in the arteries between heartbeats. One blood pressure measurement is not sufficient to diagnose hypertension. In order to be diagnosed, the child needs to have an abnormal reading on at least three visits to the doctor, and during a visit, the measurement may be taken several times to ensure it is accurate.
What is considered as “normal” blood pressure is relative and depends on the child’s gender, age and height. If hypertension is diagnosed, the child should then be checked approximately every six months. A doctor may also perform the following tests to check for other underlying conditions that may be causing the problem: Echocardiogram to check blood flow through the heart
Ultrasound to assess the kidneys Blood test to check blood cell counts, blood glucose and function of the kidneys Urine analysis Treatment Hypertension in children is generally managed by making lifestyle changes such as exercising regularly, eating a diet that is good for the heart and maintaining a healthy weight. If these measures alone are not enough to resolve the problem, medications may be prescribed.
2. Detecting Brain Disease Using the Eye. By Susha Cheriyedath, M.Sc.
The human eye shares several vascular and neural similarities to the brain, and hence, our eyes have been found to offer a direct window to brain pathology. The unique characteristics of our eyes allow them to be a relatively affordable biomarker for Alzheimer's disease (AD) and other illnesses of the brain. Currently, the diagnosis of AD is only possible after patients start showing early cognitive loss. A formal diagnosis is made using cognitive or mental state examinations, but the diagnosis can only be confirmed after examining the brain post mortem. Well-established biomarkers for AD presently used include Aβ-42, T-tau, and p-tau found in the cerebrospinal fluid, and fluorodeoxyglucose and Pittsburg Compound B found in the brain. Although these biomarkers are crucial for AD monitoring, the widespread implementation of these biomarkers is still a challenge. Visual biomarkers for AD Alzheimer's patients usually report visual symptoms, and this encouraged scientists to look for potential ocular biomarkers for AD. Studies showed that certain visual symptoms could be an indication of dementia onset as well as the development of senile plaques in the visual regions in the brain. As more and more details about the sequence of events, as well as the neurodegenerative changes in AD, are discovered, structural retinal biomarkers were found to have the potential to help in the early diagnosis of AD. Commonly reported vascular issues in AD are a blood-brain-barrier compromise, impaired Aβ clearance, vasoconstriction, reduced blood vessel density, and blood flow. Direct visualization of the hallmarks of AD in the retina can be the most promising AD biomarker because of its specificity for AD. However, ongoing work is necessary to verify that Aβ plaques are present in retinal tissues and that these retinal deposits are predictive of cerebral deposits. In addition, VVAD, a visual variant of AD, has been found to affect relatively younger people. VVAD patients present with visual symptoms in their 50s or 60s and eventually follow the course of cognitive decline typically seen in patients with AD. Non-retinal biomarkers for AD include pupillary reactions such as pupil size and pupillary response to light. Eye movements also play a crucial role because AD patients have trouble with reading due to suboptimal eye movements said to be linked to memory. AD sufferers have been shown to present with higher latency during voluntary eye movements, and show decreased eye movement speed. They may also fail to fixate on or follow a moving target. Apart from being crucial and early indicators of brain illness, these visual changes are easy to examine since the eye is very accessible, and retinal imaging is a simple procedure, all of which make ocular biomarkers very attractive.
БИЛЕТ 5 1. Can Antibiotics Increase the Risk of Arthritis? By Ratan-NM
Rheumatoid arthritis (RA) is an autoimmune disorder that causes inflammation of the joints. RA is a chronic and progressive condition that causes debilitating effects on the patient. The condition is characterized by pain and stiff joints. Another typical feature of this disorder is bone and joint destruction and the presence of autoantibodies in the serum and synovial fluid. Synovial fluid is the fluid that lubricates the synovial joints. What causes rheumatoid arthritis? The exact mechanism by which patients develop RA is unknown; however, a combination of genetic and environmental factors is likely. Autoimmune antibody production is proposed to be the main mechanism responsible for bone and joint destruction, and the related RA pathology. Infections, hormonal alterations, and stress are some potential triggers of RA.
Recent research suggests an association between antibiotic use, gut microbiota changes, and RA flares. Antibiotics and the gut microbiota Antibiotics are widely used for the treatment of bacterial infections associated with the respiratory system, gastrointestinal system, and urinary tract. Although antibiotics act against pathogenic bacteria, they can also modify the normal gut microbiota. The gut microbiota is a diverse system of microorganisms residing in the gastrointestinal tract of the human body. Gut microbiota plays a vital role in maintaining the body’s digestive health. Gut microbiota is also involved in the immune system and the synthesis of vitamin B and vitamin K. Various epidemiological studies have demonstrated associations between the occurrence of bacterial infections and RA. Furthermore, microbiome alterations have been indicated as a potential mechanism for the effect of infection in RA pathogenesis. Antibiotics substantially disturb the gut microbiome, with studies demonstrating significant microbial shifts in the gastrointestinal tract following their use. The alterations in the gut microbiome may last up to a year after treatment periods of only one week. As per a recent study by Nagra et al., the risk of RA flare was significantly increased in the 1–12 months after commencing treatment on sulphonamide and trimethoprim antibiotics. Antibiotic usage and the risk of rheumatoid arthritis Emerging research suggests that infections are potential risk factors for RA pathogenesis and flares. Respiratory infections have been particularly linked with the development of RA. Antibodies to citrullinated peptide antigens (ACPA) are one of the autoantibodies associated with RA. ACPAs have been found to be produced in response to certain bacterial components, which suggests the potential role of infections in RA pathogenesis. 2. Brain Activity During Sleep. By Yolanda Smith. Although it was historically believed that sleep was a passive but necessary process for healthy bodily functions, it is now known that brain activity continues during sleep. In fact, this brain activity is thought to play several important roles in the maintenance of physical, emotional and mental health. Brainwaves in Sleep Stages. There are different stages of sleep, each of which is characterized by unique brain activity. Stage 1 sleep is the lightest stage of sleep that occurs as an individual is falling asleep. There is slow movement of the eyes and activity of the voluntary muscles in the body is reduced. The brainwaves in stage 1 sleep are smaller and more uniform than in the awake state, what are referred to as alpha and theta waves. In stage 2 sleep, the movement of the eyes ceases and the brain waves become slower than in stage 1. There are also occasional bursts of waves that are more rapid, which are referred to as sleep spindles. Stage 3 of sleep is characterized by slow, rhythmical brain waves called delta waves. This stage of sleep is very heavy with no movement of the eyes or voluntary muscles, and it is difficult to wake a person in this stage. During REM sleep, an individual usually breathes more rapidly and there are quick movements of the eyes that characterize the state. In this stage, the brain activity is very similar to that of a person who is awake, suggesting that there are significant processes taking place in the central nervous system. REM Brain Activity. It is believed that dreaming occurs for at least 2 hours each night during REM sleep and this activity plays an important role in the processing of information and creation of memory. During this stage of sleep, heart rate and blood pressure increase and the activity of the brain is markedly more dynamic. Sleep research with EEG monitoring has established that infants spend a greater proportion of sleep time (up to 50%) in comparison to adults, leading to the hypothesis that the brain activity helps in the development of the memory and learning. The signals initiate at the base of the brain, in an area referred to as the pons, and then expand to the thalamus and cerebral cortex. The cerebral cortex is responsible for processes of learning, thinking and organizing information. Sleep Stage Cycles. Over time, an individual progresses through the different stages of sleep and the activity of the brain changes accordingly. It begins with stage 1 for about 5-10 minutes, then stage 2 for about 10 minutes, then stage 3 for about 30 minutes, before reaching REM sleep more than an hour after first falling asleep. Shortly after, the individual returns to stage 2 sleep, then stage 3 sleep and then REM sleep once again, repeating this cycle approximately five times before awakening. It is unclear why this cycling through the stages of sleep and continual changes in the brain activity is required for the healthy function of humans and other mammals. Further research in this area is currently being undertaken to understand this area more comprehensively, particularly for the function of the brain activity. БИЛЕТ 6 БИЛЕТ 7 БИЛЕТ 8 Allergies and Genetics Allergic conditions are very common in modern society and up to half of all children in the UK have been diagnosed with at least one of asthma, atopic eczema, hay fever or food allergies. With this increase in the prevalence of allergies, the development of these conditions is coming into question to help in the prevention and management.
Allergic Conditions There are several allergic conditions that are often grouped together when discussing the link between allergies and genetics, including asthma, atopic eczema, hay fever or food allergies. These conditions appear to be linked and follow a similar pattern in relation to genetic susceptibility. Children affected by allergies often follow a pattern where they will progress through a series of allergic conditions, known as the allergic march. For example, they may initially experience atopic eczema with then subsides, followed by the presentation of asthma and then rhinitis. Some children will also develop several of the allergic conditions and retain them for life Familial Link Some families appear to be more likely to be affected by allergic conditions than others and children born into these families have a higher risk of developing an allergic condition. This familial tendency to develop allergic conditions is thought to have a genetic link known as atopic. It is estimated that more than half of children born into atopic families will develop an allergic disease, whereas the incidence of children with no family history of allergic disease is one in five. The risk is elevated even further for families where both parents are affected by an allergic condition. Notably, children do not always develop the same allergic condition as the other members of the family and research tends to indicate a susceptibility to allergies, rather than a specific allergic condition. Genetic Research Genome-wide association studies (GWAS) have helped to enlighten our understanding of genes in the development of allergic conditions. Specific gene variations that alter the encoding of epithelial cell-derived cytokines such as interleukin-33 and thymic stromal lymphopoietin may be involved in the pathogenesis of allergies. Additionally, variations in the ORMDL3 and GSDML genes have been linked to an increased risk of early-onset asthma. These finding help to identify children with the highest susceptibility to allergies, which can be useful in targeting preventative techniques or being aware of allergies symptoms that require treatment. However, there remains a lot to be discovered in the research field of allergies and genetics. Further studies are required to continue broadening the understanding of the genetic development mechanisms of allergic conditions, and begin to implement techniques to lessen the impact of allergies on the modern population. БИЛЕТ 9 1. High Blood Pressure in Children. By Sally Robertson, B.Sc.
Although people usually assume that only middle-aged or elderly people develop high blood pressure (hypertension), it is also possible for the condition to arise in teenagers, children and even babies. The American Heart Association advises that all children should be checked for high blood pressure on a yearly basis, as detecting the condition and treating it early will improve the child’s health and reduce or prevent the harmful effects of the condition. Causes Hypertension in children is usually caused by another underlying health condition such as heart disease or kidney disease. Itis therefore referred to as secondary hypertension and once the medical condition is resolved, the blood pressure typically returns to normal. Secondary hypertension may also be caused by the following conditions: Hyperthyroidism Adrenal disorder Sleep problems, particularly sleep apnea Renal artery stenosis Some medications can increase blood pressure, but, again, the blood pressure usually returns to normal if the medication is discontinued. In some cases, a doctor cannot determine what is causing the hypertension, in which case the condition is referred to as primary or essential hypertension. Various factors that are known to contribute to the risk of primary hypertension include: Overweight or obesity (body mass index >25) Family history of hypertension High cholesterol and triglycerides Type 2 diabetes or raised fasting blood sugar Complications Children with hypertension often develop sleep apnea and breathe abnormally while they sleep, particularly if the child is overweight. If the hypertension persists into adulthood, the person is at an increased risk of kidney disease, stroke, heart attack and heart failure. Tests and diagnosis Blood pressure is measured using an inflatable arm cuff and blood pressure gauge. The blood pressure measurement is made up of two readings. The first (upper) number is a measurement of systolic blood pressure, which is the pressure in the arteries when the heart beats. The second (lower) number is a measurement of the diastolic pressure, which is the pressure in the arteries between heartbeats. One blood pressure measurement is not sufficient to diagnose hypertension. In order to be diagnosed, the child needs to have an abnormal reading on at least three visits to the doctor, and during a visit, the measurement may be taken several times to ensure it is accurate.
What is considered as “normal” blood pressure is relative and depends on the child’s gender, age and height. If hypertension is diagnosed, the child should then be checked approximately every six months. A doctor may also perform the following tests to check for other underlying conditions that may be causing the problem: Echocardiogram to check blood flow through the heart Ultrasound to assess the kidneys Blood test to check blood cell counts, blood glucose and function of the kidneys Urine analysis Treatment Hypertension in children is generally managed by making lifestyle changes such as exercising regularly, eating a diet that is good for the heart and maintaining a healthy weight. If these measures alone are not enough to resolve the problem, medications may be prescribed.
БИЛЕТ 10 1. Can Antibiotics Increase the Risk of Arthritis? By Ratan-NM
Rheumatoid arthritis (RA) is an autoimmune disorder that causes inflammation of the joints. RA is a chronic and progressive condition that causes debilitating effects on the patient. The condition is characterized by pain and stiff joints. Another typical feature of this disorder is bone and joint destruction and the presence of autoantibodies in the serum and synovial fluid. Synovial fluid is the fluid that lubricates the synovial joints. What causes rheumatoid arthritis? The exact mechanism by which patients develop RA is unknown; however, a combination of genetic and environmental factors is likely. Autoimmune antibody production is proposed to be the main mechanism responsible for bone and joint destruction, and the related RA pathology. Infections, hormonal alterations, and stress are some potential triggers of RA. Recent research suggests an association between antibiotic use, gut microbiota changes, and RA flares. Antibiotics and the gut microbiota Antibiotics are widely used for the treatment of bacterial infections associated with the respiratory system, gastrointestinal system, and urinary tract. Although antibiotics act against pathogenic bacteria, they can also modify the normal gut microbiota. The gut microbiota is a diverse system of microorganisms residing in the gastrointestinal tract of the human body. Gut microbiota plays a vital role in maintaining the body’s digestive health. Gut microbiota is also involved in the immune system and the synthesis of vitamin B and vitamin K. Various epidemiological studies have demonstrated associations between the occurrence of bacterial infections and RA. Furthermore, microbiome alterations have been indicated as a potential mechanism for the effect of infection in RA pathogenesis. Antibiotics substantially disturb the gut microbiome, with studies demonstrating significant microbial shifts in the gastrointestinal tract following their use. The alterations in the gut microbiome may last up to a year after treatment periods of only one week. As per a recent study by Nagra et al., the risk of RA flare was significantly increased in the 1–12 months after commencing treatment on sulphonamide and trimethoprim antibiotics. Antibiotic usage and the risk of rheumatoid arthritis Emerging research suggests that infections are potential risk factors for RA pathogenesis and flares. Respiratory infections have been particularly linked with the development of RA. Antibodies to citrullinated peptide antigens (ACPA) are one of the autoantibodies associated with RA. ACPAs have been found to be produced in response to certain bacterial components, which suggests the potential role of infections in RA pathogenesis. Лот 1 SARS-Cov-2 эволюционирует по крайней мере в течение 7 лет Д-р Лиджи Томас, доктор медицины
Нынешняя пандемия COVID-19 демонстрирует огромную неизвестность вирусологии, которая по-прежнему бросает вызов способности человечества оставаться здоровым перед лицом патогенов. В то время как большинство известных микробов имеют ограниченную близость к конкретному виду, продолжая адаптироваться к организму хозяина, коронавирус 2 с острым респираторным синдромом (SARS-Cov-2) перешел от неизвестного животного резервуара, как предыдущие SARS и MERS коронавирусы, чтобы заразить человеческие клетки. Такие вирусы, как правило, легче инфицируют и вызывают более серьезные заболевания, поскольку они еще не полностью адаптировались к целевому хозяину. Жгучий вопрос заключается в том, каким образом новые вирусы приобретают способность распознавать, связываться с клетками человека и проникать в них впервые - зависит ли это только от вирусных белков, распознающих белки клеток-хозяев, или адаптации в других вирусных процессах, которые позволяют репликацию в организме человека. Этот вопрос обсуждается исследователями Калгарийского университета в новом исследовании, опубликованном на сервере bioRxiv* в июне 2020 года. Шипованный белок является наиболее известным из белков SARS-Cov-2, и его связывание с рецепторами ACE2 на клетке-хозяине отвечает за проникновение вируса в клетку-мишень. Человеческий ACE2 (hACE2) имеет несколько редких вариантов, которые делают хозяина более уязвимым к инфекции. Аналогичным образом, белок шипа этого вируса имеет большую аффинность к рецептору, чем предыдущий SARS-вирус, что является другим возможным объяснением повышенного инфекционного потенциала текущего вируса. Последствия заключаются в том, что, во-первых, аффинность шипа-РБД к hACE2 не является основным фактором, определяющим высокую инфекционную природу нынешнего вируса, поскольку этот вирус предков был способен сделать то же самое. Во-вторых, исследователи предполагают, что этот вирус даже тогда был способен плотно связываться с рецептором. Поэтому этого недостаточно для получения наблюдаемой в настоящее время способности к быстрому и широкому распространению среди людей. Вместо этого, это должно быть связано с другим набором мутаций в вирусном геноме. Ещё одним последствием является то, что нынешний вирус, возможно, вообще не перешел на людей животного происхождения, потому что его близость к hACE2 не была недавно приобретённой молекулярной особенностью. Это может означать, что способность заражать человеческие клетки существовала в течение более продолжительного периода времени в прошлом, но вызывала менее очевидные или меньшие клинические симптомы, которые прошли незамеченными. Другая альтернатива заключается в том, что она затрагивает лишь небольшое число людей, позволяя ей оставаться в поле зрения общественного здравоохранения.
|
|||||||||
|
Последнее изменение этой страницы: 2021-04-12; просмотров: 58; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 3.17.165.168 (0.136 с.) |