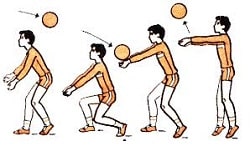
Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
History of the injury and description of the patient's symptoms
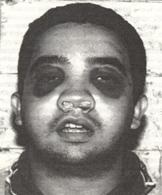
If the patient is unconscious or confused, any relevant facts concerning the accident and the subsequent management of the patient must be obtained from eye-witnesses, ambulance persons, or medical and dental practitioners who may have attended the patient following the injury. If the patient is conscious and co-operative a history can be obtained, but as patients with facial injuries may experience some difficulty in talking owing to the discomfort and mobility of the fractures the interrogation should be brief at this stage: 1. Loss of consciousness: It is essential to ask if loss of consciousness has occurred and, in that event, whether the patient can remember up to the moment of the accident or whether there is a memory gap. Pre-traumatic or anterograde amnesia is failure to remember up to the time of injury and post-traumatic or retrograde amnesia is loss of memory following the accident - both are indicative of cerebral damage. 2. Symptoms: It is also important to enquire whether the patient has any difficulty in breathing or swallowing and whether he or she has a headache or pain elsewhere in the body. 3. Medication: If possible all current medication should be recorded. Information as to whether the patient was being treated with insulin, steroids or anticoagulants prior to the accident is particularly important. 4. Consumption of food or drink: Recent alcohol consumption and a history of recent food intake should be obtained from either the patient or accompanying persons. A detailed history is obtained when the patient can talk more comfortably. Local clinical examination of the facial injury The examination of a patient with a recent severe injury to the facial skeleton will be greatly facilitated if the patient's face is gently washed with warm water and cotton-wool swabs to remove caked blood. The congealed blood in the palate and buccal sulcus can be removed with cotton wool held in non-toothed forceps. Sometimes cotton-wool swabs dipped in hydrogen peroxide will facilitate the removal of any particularly tenacious clots in the mouth and upon the teeth. If a denture is fractured, the fragments should be assembled to make sure that no portion is missing - possibly displaced down the throat. Only after careful cleaning has been carried out, both extra-orally and intra-orally, is it possible to evaluate the full extent of the injury. It is surprising how often the magnitude of the surgical problem diminishes as the overlying blood is removed and accurate visualization becomes possible. External examination The operator should take careful note of oedema, ecchymosis and soft-tissue lacerations. Any obvious bony deformities, haemorrhage or cerebrospinal fluid leak should be recorded. Many of the physical signs of a fractured bone result from the extravasation of blood from the damaged bone ends. This results in rapid early swelling from the accumulation of blood within the tissues and subsequent even greater swelling resulting from increased capillary permeability and oedema. Swelling and ecchymosis often indicate the site of individual fractures, particularly of the mandible or zygoma. There may be obvious deformity in the bony contour of the mandible, and if considerable displacement has occurred the patient is unable to close the anterior teeth together and the mouth hangs open. A conscious patient may seek to support the lower jaw with his hand. Many fractures are compound into the mouth and blood-stained saliva is frequently observed dribbling from the corners of the mouth, particularly if the fracture is recent. The eyelids are gently separated and, if the patient is conscious, visual acuity is tested in each eye. The patient is asked to follow the clinician's finger with his or her eyes and to report if diplopia occurs. A note is made of any alteration in the size of the two pupils, and the light reflex is tested. The extent of any sub-conjunctival ecchymosis is recorded (see below).
Gentle palpation should begin at the back of the head, and the cranium should be explored for wounds and bony injuries. The fingers should then be run lightly over the zygomatic bones and arch, and around the rim of the orbits. Areas of tenderness, step deformities, and unnatural mobility are noted. The nasal complex is next examined in the same manner. Palpation should continue bilaterally in the condylar region and continue downwards and along the lower border of the mandible. Bone tenderness is almost pathognomonic of a fracture, even an undisplaced crack, but if there is more displacement it may be possible to palpate deformity or elicit bony crepitus. Areas of loss of skin sensation should be noted. The infraorbital nerve is frequently contused when the zygomatic complex has been fractured producing anaesthesia or paraesthesia of the cheek, lateral aspect of the nose, and half of the upper lip. Fractures of the body of the mandible are often associated with injury to the inferior dental nerve, in which case there will be reduced or absent sensation on one or both sides of the lower lip. Intra-oral examination It is impossible to assess intra-oral damage if the parts are obscured by blood. Conscious cooperative patients may be given a lukewarm mouthwash but in most cases the clinician will have to remove the clotted blood by gently cleaning the whole area with moistened swabs. Congealed blood and any fragments of teeth, alveolus or dentures are removed carefully by forceps, assisted by gentle suction if available. A good light is essential. The buccal and lingual sulci are examined for ecchymosis. Sub-mucosal extravasation of blood is often indicative of underlying fracture, particularly on the lingual side. Ecchymosis in the buccal sulcus is not necessarily the result of a fracture as there is considerable soft tissue overlying the bone in this area and extensive bruising may follow a blow insufficient to cause a fracture. However, on the lingual side the mucosa of the floor of the mouth overlies the periosteum of the mandible which, if breached following a fracture, will invariably be the cause of any leakage of blood into the lingual submucosa. This then is a most valuable sign of bony injury in the body of the mandible. Small linear haematomas, particularly in the third molar region, are reliable indicators of adjacent fracture. The mucosa overlying the root of the zygoma should be carefully examined as fractures of the zygomatic complex and Le Fort I fractures frequently produce a haematoma in this area. A haematoma in the palate is a reliable sign of a bony split associated with a fracture of the mid-face. The occlusion of the teeth is next examined or, if the patient is edentulous, the alveolar ridge. Premature contact of the posterior teeth with defects in the occlusion or alveolus are noted along with any obvious lacerations of the overlying mucosa. It is important to examine all the individual teeth and to note any luxation or subluxation along with missing crowns, bridges or fillings. Individually fractured teeth must be assessed for involvement of the dentine or pulp. Finally, all teeth should be carefully examined with a mirror and probe to detect loose fillings, fine cracks or splits in the tooth substance. If teeth, portions of teeth, dentures, fillings, etc. are not accounted for, a radiograph of the chest must be ordered in case they have been inhaled. Possible fracture sites in the mandible are gently tested by placing a finger and thumb on each side and using pressure to elicit unnatural mobility. If the patient can co-operate, he or she is asked to carry out a full range of mandibular movements and any pain or limitation of movement recorded. Occasionally, even this detailed examination fails to confirm a mandibular fracture which is thought to be present from the history and presence of haematoma. In such cases the flat of both hands should be placed over the two angles of the mandible and gentle pressure exerted. This manoeuvre will always elicit pain when even a crack fracture is present, but the procedure should be one of last resort as it produces extreme discomfort if a mobile fracture is present.
In the upper jaw the tooth-bearing segment is gently manipulated to elicit unnatural mobility. A finger and thumb are then placed over the frontonasal suture line and any mobility of the facial skeleton tested by pressure from the fingers in the palate. A false impression of mobility of the mid-facial skeleton can be obtained, especially in the unconscious patient, by pressure in the palate alone, for the upper part of the head moves inside the epicranial aponeurosis producing the illusion of movement of the mid-facial skeleton. If the dento-alveolar segment moves independently of the remainder of the mid-facial skeleton, particularly if crepitus is elicited, it is indicative of a Le Fort I type fracture. The upper teeth should be tapped with the handle of a dental mirror. A characteristic «cracked-pot» sound is elicited if there is a fracture above the teeth. 6. MATERIALS FOR SELF-CONTROL: A. Questions for self-control: Symptom of glasses at fracture of maxilla
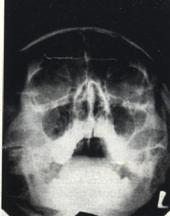
Direct and lateral projection of facial bones.
Axial and semi-axial projection of skull.
Lateral projection of mandible.
B. Tasks for self-control: 1. The patient asked to the doctor with the trauma of the nose, resulting in sports training. After examination doctor diagnosis nasal bone fracture without displacement of fragments. How to classify this injury etiology, given that the patient worked as a sports coach? (Answer: work injury). 2. Worker got hit the board in the region of upper jaw during the home renovation at the weekend. Doctor diagnosis contused wound of the upper lip, partial dislocation of the maxillary incisors. Qualify as an injury received in such circumstances? (Answer: consumer injury). 3. The patient complained of pain and impaired chewing due blow to the angle of the lower jaw to the right, headache, nausea. Set a preliminary diagnosis of fracture of the lower jaw. What additional studies should be carried out for the diagnosis? (Answer: X-ray, consultation neurologist). C. Materials for test control. Test tasks with the single right answer (a=II): 1. What damage is izolated? A. Burn of face and neck. B. Fracture of maхilla and mandible. C. Fracture of mandible. D. Wound of check and inframandible area. E. Fracture of nose and concussion of cerebrum. (Correct answer: С). 2. What damage is combined? A. Wound of check. B.Wound of chine. C. Fracture of nose and concussion of cerebrum. D. Fracture of maхilla and mandible. E. Fracture of mandible and termical burn of face. (Correct answer: Е). D. Educational tasks of 3 th levels (atypical tasks): 1. A patient with an open fracture of the body of the mandible is brought to Maxillofacial department from the place of accident. The general state of the patient is moderate severity, at anamnesis of desease: unconsciousness for a few minutes and vomiting. The patient complains of nausea, weakness, pain in the left side of the abdomen. Blood pressure – 100/60 mm Hg. Art., pulse 100 beats / min., weak filling. Under the block anesthesia maxillo-facial surgeon produced reposition of fragments and fiхated their by Tigershtedt’s tires with toe loops, and then appointed a consultation of therapists. Find the mistakes in the actions of the doctor: (Answer: the victim have the complex trauma with signs of traumatic shock, in this state surgery manipulation performed due bleeding or asphyxia only, should be consultation of surgeon traumatologist and a neurologist). 2. The patient complains of pain in the angle of the lower jaw at chewing, headache, dizziness, nausea. It is established that the patient was beaten 24 hours ago, there was a loss of consciousness for a few minutes. After clinical and radiographic examination, the doctor ruled out the diagnosis of a fracture of the lower jaw, doctor appointed Ketanov and inspected in 3 days. What is wrong in the actions of the doctor. (Answer: at this clinical picture neurologist consultation was necessary). 3. At examination of the victim dentist diagnosis bilateral fracture of the lower jaw in the chin with a displacement of bone fragments. After that doctor perfomed pressing bandage for transport immobilization. During transport, the patient showed signs of respiratory disorders. What type of asphyxia occurred in the patient and what is wrong in the actions of the doctor? (Answer: compressive bandage is contraindicated in fractures of the lower jaw with displacement, as it leads to further displacement of bone fragments. This patient had dislocation asphyxia).
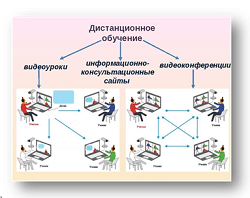
Theme 2. SUBJECT AND GOALS OF MILITARY STOMATOLOGY. ORGANIZATION OF SURGICAL AID FOR MAXILLOFACIAL VICTIMS AT PEACE TIME AND EXTREME CONDITIONS. MILITARY-MEDICAL DOCTRINE. GENERAL PRINCIPLES OF ORGANIZATION, CONTENT AND RENDERING OF MEDICAL AID, STAGES OF MEDICAL EVACUATION AND MEDICAL SCREEN OF WOUNDED IN MAXILLOFACIAL AREA. 3. ACTUALITY OF THEME: The military stomatology is a section of the military medicine which task is the organization and granting all types of the stomatologic aid to staff of Armed forces of Ukraine in the conditions of peace and a war time. Knowledge of features of gunshot and not gunshot wounds, diseases of tissues and bodies of a maxillofacial site, the organization of medical care, prevention of complications and treatment wounded in the conditions of extreme situations and a war time - a direct duty of the stomatologist. The knowledge of the principles of medical sorting, volume of medical care at stages of medical evacuation of the wounded will allow the stomatologist to organize rationally providing medical care to the maxillofacial wounded. 2. СONCRETE AIMS: 1.1. To analyze provisions of the military-medical doctrine in historical aspect. 1.2. To explain basic provisions of the military-medical doctrine. 1.3. To offer forces and means of a health service for rendering the stomatological surgical aid to wounded in maxillofacial area. 1.4. To classify the basic principles of the organization, content and rendering of medical aid at stages of medical evacuation by the wounded in maxillofacial area. 1.5. To treat basic provisions of a medical deontology and medical ethics at assistance to wounded in maxillofacial area. 1.6. To draw the scheme of medical screen of wounded in maxillofacial area. 1.7. To analyze the principles of medical screen of wounded in maxillofacial area. 1.8. To make the scheme of medical evacuation of wounded in maxillofacial area. 3. BASIC KNOWLEDGE, ABILITIES, SKILLS, WHICH are NECESSARY FOR STUDY THEMES (intradisciplinary integration).
|
||||||
|
Последнее изменение этой страницы: 2021-01-08; просмотров: 86; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 3.141.193.158 (0.009 с.) |