Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь FAQ Написать работу КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
Drug-Laboratory Test InteractionsСодержание книги
Поиск на нашем сайте
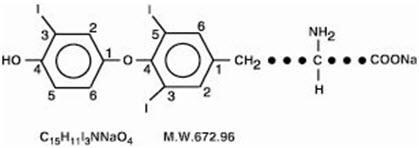
Consider changes in TBG concentration when interpreting T4 and T3 values. Measure and evaluate unbound (free) hormone in this circumstance. Pregnancy, infectious hepatitis, estrogens, estrogen-containing oral contraceptives, and acute intermittent porphyria increase TBG concentrations. Nephrosis, severe hypoproteinemia, severe liver disease, acromegaly, androgens and corticosteroids decrease TBG concentration. Familial hyper- or hypo-thyroxine binding globulinemias have been described, with the incidence of TBG deficiency approximating 1 in 9000. USE IN SPECIFIC POPULATIONS Pregnancy Risk Summary Experience with liothyronine use in pregnant women, including data from post-marketing studies, have not reported increased rates of major birth defects or miscarriages (see Data). There are risks to the mother and fetus associated with untreated hypothyroidism in pregnancy. Since TSH levels may increase during pregnancy, TSH should be monitored and CYTOMEL dosage adjusted during pregnancy (see Clinical Considerations). There are no animal studies conducted with liothyronine during pregnancy. CYTOMEL should not be discontinued during pregnancy and hypothyroidism diagnosed during pregnancy should be promptly treated. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Clinical Considerations Disease-associated maternal and/or embryo/fetal risk Maternal hypothyroidism during pregnancy is associated with a higher rate of complications, including spontaneous abortion, gestational hypertension, pre-eclampsia, stillbirth, and premature delivery. Untreated maternal hypothyroidism may have an adverse effect on fetal neurocognitive development. Dose adjustments during pregnancy and the postpartum period Pregnancy may increase CYTOMEL requirements. Serum TSH levels should be monitored and the CYTOMEL dosage adjusted during pregnancy. Since postpartum TSH levels are similar to preconception values, the CYTOMEL dosage should return to the pre-pregnancy dose immediately after delivery [see Dosage and Administration (2.3)]. Data Human Data Liothyronine is approved for use as a replacement therapy for hypothyroidism. Data from post-marketing studies have not reported increased rates of fetal malformations, miscarriages, or other adverse maternal or fetal outcomes associated with liothyronine use in pregnant women. Lactation Risk Summary Limited published studies report that liothyronine is present in human milk. However, there is insufficient information to determine the effects of liothyronine on the breastfed infant and no available information on the effects of liothyronine on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for CYTOMEL and any potential adverse effects on the breastfed infant from CYTOMEL or from the underlying maternal condition. Pediatric Use The initial dose of CYTOMEL varies with age and body weight. Dosing adjustments are based on an assessment of the individual patient's clinical and laboratory parameters [see Dosage and Administration (2.3, 2.4)]. In pediatric patients in whom a diagnosis of permanent hypothyroidism has not been established, discontinue thyroid hormone for a trial period, but only after the child is at least 3 years of age. Obtain serum TSH, T4, and T3 levels at the end of the trial period, and use laboratory test results and clinical assessments to guide diagnosis and treatment, if warranted [see Dosage and Administration (2.6)]. Congenital Hypothyroidism [see Dosage and Administration (2.2, 2.6)] Rapid restoration of normal serum T4 concentrations is essential for preventing the adverse effects of congenital hypothyroidism on intellectual development as well as on overall physical growth and maturation. Therefore, initiate thyroid hormone immediately upon diagnosis. Thyroid hormone is generally continued for life in these patients. Closely monitor infants during the first 2 weeks of thyroid hormone therapy for cardiac overload, arrhythmias, and aspiration from avid suckling. Closely monitor patients to avoid undertreatment or overtreatment. Undertreatment may have deleterious effects on intellectual development and linear growth. Overtreatment is associated with craniosynostosis in infants, may adversely affect the tempo of brain maturation, and may accelerate the bone age and result in premature epiphyseal closure and compromised adult stature [see Dosage and Administration (2.6) and Adverse Reactions (6)]. Acquired Hypothyroidism in Pediatric Patients Closely monitor patients to avoid undertreatment and overtreatment. Undertreatment may result in poor school performance due to impaired concentration and slowed mentation and in reduced adult height. Overtreatment may accelerate the bone age and result in premature epiphyseal closure and compromised adult stature. Treated children may manifest a period of catch-up growth, which may be adequate in some cases to normalize adult height. In children with severe or prolonged hypothyroidism, catch-up growth may not be adequate to normalize adult height [see Adverse Reactions (6)]. Geriatric Use Because of the increased prevalence of cardiovascular disease among the elderly, initiate CYTOMEL at less than the full replacement dose [see Dosage and Administration (2.3) and Warnings and Precautions (5.1)]. Atrial arrhythmias can occur in elderly patients. Atrial fibrillation is the most common of the arrhythmias observed with thyroid hormone overtreatment in the elderly. OVERDOSAGE The signs and symptoms of overdosage are those of hyperthyroidism [see Warnings and Precautions (5.4) and Adverse Reactions (6)]. In addition, confusion and disorientation may occur. Cerebral embolism, seizure, shock, coma, and death have been reported. Symptoms may not necessarily be evident or may not appear until several days after ingestion. Reduce the CYTOMEL dose or temporarily discontinued if signs or symptoms of overdosage occur. Initiate appropriate supportive treatment as dictated by the patient's medical status. For current information on the management of poisoning or overdosage, contact the National Poison Control Center at 1-800-222-1222 or www.poison.org. DESCRIPTION CYTOMEL tablets contain the active ingredient, liothyronine (L-triiodothyronine or LT3), a synthetic form of a thyroid hormone liothyronine in sodium salt form. It is chemically designated as L-Tyrosine, O-(4-hydroxy-3-iodophenyl)-3,5-diiodo-, monosodium salt. The molecular formula, molecular weight and structural formula of liothyronine sodium are given below.
CYTOMEL tablets contain liothyronine sodium equivalent to liothyronine in 5 mcg, 25 mcg, and 50 mcg. Inactive ingredients consist of calcium sulfate, corn starch, gelatin, stearic acid, sucrose and talc. CLINICAL PHARMACOLOGY Mechanism of Action Thyroid hormones exert their physiologic actions through control of DNA transcription and protein synthesis. Triiodothyronine (T3) and L-thyroxine (T4) diffuse into the cell nucleus and bind to thyroid receptor proteins attached to DNA. This hormone nuclear receptor complex activates gene transcription and synthesis of messenger RNA and cytoplasmic proteins. The physiological actions of thyroid hormones are produced predominantly by T3, the majority of which (approximately 80%) is derived from T4 by deiodination in peripheral tissues. Pharmacodynamics The onset of activity of liothyronine sodium occurs within a few hours. Maximum pharmacologic response occurs within 2 or 3 days. Pharmacokinetics Absorption T3 is almost totally absorbed, 95 percent in 4 hours. The hormones contained in the natural preparations are absorbed in a manner similar to the synthetic hormones. Distribution Liothyronine sodium (T3) is not firmly bound to serum protein. The higher affinity of levothyroxine (T4) for both thyroid-binding globulin and thyroid-binding prealbumin as compared to triiodothyronine (T3) partially explains the higher serum levels and longer half-life of the former hormone. Both protein-bound hormones exist in reverse equilibrium with minute amounts of free hormone, the latter accounting for the metabolic activity. Elimination Metabolism The major pathway of thyroid hormone metabolism is through sequential deiodination. Approximately 80% of circulating T3 is derived from peripheral T4 by monodeiodination. The liver is the major site of degradation for both T4 and T3. T3 is further deiodinated to diiodothyronine. Thyroid hormones are also metabolized via conjugation with glucuronides and sulfates and excreted directly into the bile and gut where they undergo enterohepatic recirculation. Excretion Thyroid hormones are primarily eliminated by the kidneys. A portion of the conjugated hormone reaches the colon unchanged and is eliminated in the feces. The biological half-life is about 2–1/2 days. NONCLINICAL TOXICOLOGY
|
||||
|
Последнее изменение этой страницы: 2019-04-27; просмотров: 161; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 18.117.151.127 (0.008 с.) |