Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
Non-compression small plates
Small conventional orthopaedic plates have been used in the past for the treatment of mandibular fractures. These plates are, however, larger than the presently designed miniplates and offer no advantages (Fig. 3). The only reason for using a plate of larger dimension than the miniplates is to incorporate compression across the fracture.
Figure 3. A standard non-compression orthopaedic plate which was removed from a treated fracture of the angle of the mandible. Insertion and removal required a large extra-oral submandibular incision.
Compression plates Compression osteosynthesis of mandibular fractures is based on the firm biological principles established for the treatment of fractures of weight-bearing long bones. However, as has been previously pointed out, non-union or delayed union is rarely a problem in fractures of the mandible or other facial bones. On the other hand, precise reduction is essential in the dentate mandible and precise reduction is difficult to achieve with compression plating techniques. It is probably true to say that compression plates have now been abandoned by the majority of maxillofacial treatment centres. For the student it is instructive to examine why this has occurred. Mandibular compression plates are either AO dynamic compression plates or plates based on the same design principle. For anatomical reasons it is necessary to apply these plates to the convex surface of the mandible at its lower border. However skilfully the plate is adapted there is a tendency for the upper border and the lingual plate to open with the final tightening of the screws. This leads both to distortion of the occlusion and, in a bilateral fracture, to opening of the fracture line on the other side (Spiessl, 1972). In order to overcome these problems various designs of compression plate were devised (Prein and Kellman, 1987). Unlike miniplates (see below) these are often applied to the bone surface using screws which engage the inner cortical plate and must therefore be sited below the inferior dental canal. All compression plates include at least two pear-shaped holes. The widest diameter of the hole lies nearest the fracture line. The screw is inserted in the narrow part of the hole and at the final moment of tightening its head slides forcibly into the wider diameter section, which is countersunk to receive it (Fig. 4).
Figure 4. Diagrammatic representation of a small compression plate to illustrate the principle by which compression of the bone interface is achieved. The eccentric pear-shaped holes in the plate cause inward movement of the screw at the final stage of tightening when the head of the screw localizes in the wider part of the pear-shaped hole.
The compression holes in the plate may be positioned one on each side of the fracture (Spiessl, 1972) or both on the same side (Becker, 1974). Because of the tendency for the upper border to open when compression is applied across the fracture at the lower border, it is necessary to apply a tension band at the level of the alveolus before tightening the screws (Figs. 5 and 6). This can be in the form of an arch bar ligatured to the teeth or as a separate plate with screws penetrating the outer cortex only. Schilli (1977) designed a plate with oblique lateral holes which ensured that the compressing force was in part directed towards the upper border so that when the plate was tightened into place there was less tendency for the fracture line to gape. Raveh et al. (1987) employed a special adjustable temporary plate at the upper border which enabled them to achieve precise reduction of the fracture prior to application of the definitive lower border dynamic compression plate. They found no application for the eccentric dynamic compression plate in their large series of cases and reported malocclusion post-reduction in only 0.5 per cent of patients. Other workers have either placed the patient in temporary intermaxillary fixation or employed special adjustable bone-holding forceps to ensure accurate fracture reduction prior to application of the compression plate.
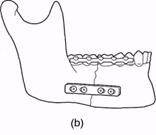
It has become increasingly apparent that compression plates offer no material advantage to the patient in the treatment of facial bone fractures. The operative approach tends to be lengthy and requires considerable expertise to produce consistent results. This is especially so if an intra-oral approach is used or if preliminary intermaxillary fixation is applied. Compression plating becomes more difficult when there is any obliquity of the fracture because of the depth of penetration of the screws. Problems also arise when there is comminution at the lower border, which is not always apparent from conventional radiographs. Perhaps the chief disadvantage, however, is the actual bulk volume of the fixation plate, which necessitates later removal in a high proportion of patients. This, of course, means subjecting the patient to a further general anaesthetic not otherwise indicated. For all of these reasons the majority of surgeons now use non-compression miniplates exclusively. Miniplates Roberts (1964) used cobalt-chrome alloy meta-carpal plates up to 1 inch (2.5 cm) in length to treat a series of mandibular fractures. These were applied to the outer cortical plate after reduction of the fracture, by means of 7 mm long screws 1.5 mm in diameter. Roberts later designed plates specifically for mandibular plating. Battersby (1966) subsequently reviewed a series of 350 cases treated in this way over a 12-year period and demonstrated satisfactory fixation. The plates were, however, employed as an alternative to transosseous wiring and most patients needed to be placed into intermaxillary fixation as well. Michelet and Moll (1971) described the use of similar small cobalt-chrome alloy plates of various lengths, and subsequently Michelet et al. (1973) reported results in 300 cases. These chrome-cobalt alloy plates were difficult to adapt and were not widely adopted. Champy et al. (1978) introduced a miniplate system customized for use in mandibular fractures. Originally fashioned in stainless steel, similar plates have now become widely available made from titanium (Figs. 89 and 94). Champy and his co-workers argued that compression plates were unnecessary because there was a natural line of compression along the lower border of the mandible. They further claimed that compression exerted a stress-shielding effect which was detrimental to ultimate mandibular strength. Non-compression miniplates with screw fixation confined to the outer cortex allow the operator to place plates both immediately sub-apically as well as at the lower border. The stress distribution after fracture of the body of the mandible has been investigated using stressed bars of epoxy resin to simulate the fractured mandible. On the basis of these studies it is suggested that fractures at the angle can be secured with a single plate as near to the upper border as the dental anatomy permits. In the canine region two plates are ideally required, one juxta-alveolar and one at the lower border. All plates can be inserted by an intra-oral approach without the need for intermaxillary fixation (Fig. 7).
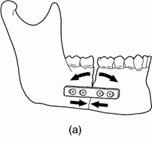
Figure 5. Diagram illustrating the chief problem with a compression plate, (a) Compression near the lower border opens up the fracture at the alveolar margin, (b) A tension band previously applied to the teeth prevents the distorting effect of the lower border compression plate, (c) A similar effect is achieved by prior application of a small cortical non-compression plate above the level of the inferior.
Figure 6. Radiographs showing the use of a compression plate at the lower border in conjunction with a non-compression cortical plate above the level of the inferior dental canal. (Case treated by Professor J. Prein and reproduced with his kind permission).
Figure 7. (a) The post-traumatic occlusion of a patient with a bilateral fracture of the body of the mandible. The 'step' deformity in the left mandible is clearly illustrated, (b) Postero-anterior radiograph showing fractures in the right molar and left canine regions of the mandible, (c) Operative photograph showing a non-compression miniplate applied across the fracture in the right retromolar region, (d) Operative view of the left canine region. The fracture was reduced with the aid of a temporary wire around the teeth. Two cortical miniplates have been inserted taking care to avoid damage to the mental nerve, which is shown emerging from the mental foramen. Miniplates of this design are now widely used and reported results are encouraging. The operative time involved is no more than that required for transosseous wiring. Cawood (1985) compared 50 cases treated by conventional intermaxillary fixation with 50 cases treated by miniplates. The plated series had a higher incidence of residual malocclusion (8%) but there were no cases of delayed union compared with 6 per cent in the control group. Of the plated cases 6 per cent became infected compared with 4 per cent of the controls and 3.8 per cent in a comparable group treated in an independent hospital department. Postoperative infection of miniplates appears to vary considerably from unit to unit. Wald et al. (1988) have reviewed the literature and report complications as high as 30 per cent in some series. The risk of infection from various plating systems has been reviewed by Ellis (1999). Miniplate osteosynthesis can be used in virtually all types of mandibular body fracture. Plates can be inserted via an intra-oral approach using special cheek retractors and protective sleeves passed through the soft tissues of the cheek. It is only necessary to reflect periosteum from the outer plate of bone, which is an advantage when compared with transosseous wiring. A few surgeons favour the use of simultaneous intermaxillary fixation when using miniplates (Mommaerts and Engelke, 1986). The plates can usually be left in permanently without causing trouble (Haug, 1996), but on theoretical grounds Cawood (1985) recommends removal because of the continuing effect on the functional forces within the bones. There is also now firm evidence that corrosion and local dispersal of titanium does take place but this is only detectable by ultramicroscopic techniques (Kim et al., 1997). The significance in the long term cannot yet be evaluated, which is regarded by some as an indication for removal of all plates (Haers et at., 1999). Lag screws A few oblique fractures of the mandible can be rigidly immobilized by inserting two or more screws whose thread engages only the inner plate of bone. The hole drilled in the outer cortex is made to a slightly larger diameter than the threaded part of the screw. When tightened the head of the screw engages in the outer plate and the oblique fracture is compressed. At least two such lag screws are necessary to achieve rigid immobilization (Fig. 8). The technique has been well reviewed by Leonard (1987).
Figure 7. (continued) (e) Postoperative radiograph. The fractures have been satisfactorily reduced and immobilized by non-compression miniplates. (f) Immediate postoperative photograph of the occlusion. The temporary wire ligature around the teeth on each side of the left mandibular body fracture has not yet been removed.
|
||||||||||||||||||||||||||||||||||||||
|
Последнее изменение этой страницы: 2021-01-08; просмотров: 228; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 18.223.134.29 (0.008 с.) |
|||||||||||||||||||||||||||||||||||||||