
Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
Osteosynthesis without intermaxillary fixation
This can only regularly be achieved by some form of bone plate although some oblique fractures can be fixed by the application of suitably positioned lag screws. Currently, three main systems of bone plating are used for fixation of mandibular fractures. Small bone plates based on the Swiss AO system (Arbeitsgemeinschaft fur Osteosynthese) and the ASIF technique (Association for the Study of Internal Fixation) are designed for compression (Raveh et al., 1987). An example of a small compression plate is shown in Fig. 1, but plates of similar dimensions can equally be of simple non-compression design. The main alternative which has found favour has been the use of miniaturized plates such as those originally used for injuries to the fingers (Hayter and Cawood, 1993) (Fig. 2). All forms of bone plating provide rigid fixation. However, a distinction should be made between semi-rigid plates and compression plates. In the former group a small gap between the bone ends exists which means that a limited amount of primary callus forms, whereas, when compression plates are used, experimental evidence suggests that primary bone healing takes place without the formation of any intermediate callus. It is claimed that the full strength of the bone is thereby restored more rapidly. Each system ensures sufficient rigidity across the fracture site to obviate the need for intermaxillary fixation. This enables the patient to enjoy a relatively normal diet and to maintain oral hygiene more easily. These conditions are desirable for all mandibular fractures but there are particular clinical indications in certain cases. For example, a fracture of the body of the mandible with a coexistent intracapsular fracture of the condyle may make early mobilization especially important to order to ensure recovery of function of the temporo-mandibular joint. Again, intermaxillary fixation is not well tolerated in some elderly patients and is particularly difficult to maintain in mentally disturbed or subnormal individuals. However, the application of bone plates to the mandible is an exacting technique requiring a fairly long period of general anaesthesia and a considerable degree of surgical skill. Many surgeons routinely still use an extra-oral approach which leaves a scar on the face at the conclusion of treatment. Plating is increasingly carried out from an intra-oral approach but the technique requires special surgical instruments in order to gain access to all areas of the body of the mandible. Becker (1974) has pointed out that any treatment method which does not rely on intermaxillary fixation must ensure the restoration and maintenance of correct occlusion. In spite of numerous claims to the contrary, bone plates because of their very precision do not always achieve this fundamental objective. The occlusal problem can be overcome in skilled hands. Raveh et al. (1987) have reported results in 531 mandibular fractures treated with AO plates followed by immediate mobilization. All cases were operated on via an intra-oral approach and only two cases exhibited mal-occlusion. This group employed a special localization device across the fracture line, which was inserted and adjusted prior to the placement of the plate. In other series, however, up to 25 per cent of cases treated required some adjustment by occlusal grinding, and to avoid this patients treated by plating techniques may need to be placed into intermaxillary fixation for a significant period (Pogrel, 1986). Plates are particularly useful in patients who are either partially or completely edentulous.
Figure 1. A compression bone plate. In this design both of the 'pear'-shaped compression holes are to the left of the fracture line. (Case treated by Mr P. T. Blenkinsopp and reproduced with his kind permission).
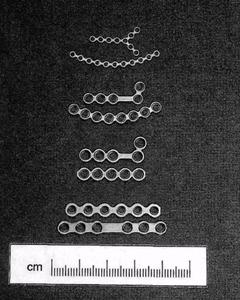
Figure 2. (a) A miniaturized plating system based on the original design by Professor M. Champy. The 2 mm and 1.5 mm systems are shown, (b) Individual plate design from the AO miniaturized plating system showing, from above down, pairs of 1 mm microplates, 1.5 mm compact plates, 2.0 mm compact plates and stronger 2 mm mandibular plates.
The incidence of postoperative infection of bone plates seems to be decreasing and compares favourably with other methods of fixation. Plating may indeed be employed for the elective treatment of infected fractures (Koury et al., 1994) although the incidence of persistent infection postoperatively is higher than in non-infected cases. Some of these improved results can be attributed to greater surgical skill and some to the use of more biocompatible materials. Titanium has now replaced stainless steel and chrome-cobalt alloys for the manufacture of all types of plates. There is no convincing evidence to challenge the biocompatibility of titanium bone plates, nor is there a need for them to be removed electively. Most surgeons throughout the world leave asymptomatic plates in situ (Haug, 1996). Nevertheless, a few plates have to be removed due to later infection (Souyris et al., 1980), and in a number of centres patients are routinely readmitted for elective removal (Alpert and Seligson, 1996). There are certainly theoretical reasons for removal of metal plates on the grounds that they protect the underlying bone from normal stress and therefore lead to atrophic changes Metal will also cause artefacts on postoperative computed tomography (CT) and magnetic resonance imaging (MRI). There is now evidence that titanium is not quite as biologically inert as was originally supposed. Limited corrosion takes place with detectable particles in both local tissue and regional lymph nodes These findings have reinforced the arguments for routine removal of all metal plates. This in turn begs the question that if all plates are to be removed why use an expensive material like titanium rather than stainless steel? For all of these reasons maxillofacial surgeons as well as orthopaedic surgeons have looked for a biodegradable material which could be used for the construction of bone plates of sufficient strength and acceptable bulk to satisfy the mechanical requirements of both craniofacial reconstruction and the management of facial fractures. The most obvious available material is bone itself, either autogenous or bank. Records of individual patients from World War I describe the use of screws and dowels fashioned from bone which were used to fix mandibular fractures and bone grafts in an effort to avoid the ever-present risk of infection. More recently, Obwegeser (1997) has described a bioconvertible osteosynthesis system utilizing plates and screws made from autogeneic or allo-geneic cortical bone and which has been in clinical use since 1992. There is a distinction between materials that are biodegradable, i.e. are broken down within the body, and those which are bioabsorbable, i.e. are completely eliminated. Lindqvist and his co-workers in Helsinki have extensively investigated bioabsorption and the use of bioabsorbable materials in maxillofacial surgery (Lindqvist, personal communication; Suuronen et al., 1999). Research has concentrated latterly on a group of high molecular weight poly-alpha-hydroxy acids and their copolymers -specifically polylactic acid (PLA), polyglycolic acid (PGA) and polydioxanone (PDS). Initially the laevo form of polylactic acid showed most promise. The mechanical properties were substantially improved by two further developments. It was found that copolymers of laevo-and dextro-lactic acid in certain proportions could be formed into small plates which were heat-malleable, resorbed within 2 years and were strong enough for craniofacial reconstruction. The material was still not sufficiently robust to be used for most mandibular fractures. A second important development took place when it was discovered that the polymer elements could be orientated during manufacture to strengthen the final product even more - a process of self-reinforcement. Self-reinforced copolymer can be bent and adapted at room temperature using suitable pliers, and can be sterilized by gamma radiation. The most promising present material is, accordingly, a self-reinforced copolymer of l- and DL-lactide which can be fashioned into miniplates. They are already widely used for craniofacial and orthognathic surgery but whether they have sufficient strength for the routine treatment of fractures of the mandible is less certain (Tarns et al, 1999). At their present stage of development bioabsorbable plates and lag screws appear to have a place in the fixation of fractures of the mandibular symphysis where there is good bony contact.
|
||||||||
|
Последнее изменение этой страницы: 2021-01-08; просмотров: 69; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 3.21.76.0 (0.008 с.) |

 (a)
(a)
 (b)
(b)



