Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
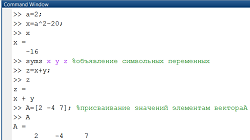
Some Medications that Cause Changes in Urine Color.Стр 1 из 4Следующая ⇒
EXAMINATION OF URINE. URINALYSIS (UA; routine UA) is an important routine screening test that gives information about the status of the renal and urinary tracts and the total body system. The test involves collection of a random sample of at least 100-200 ml of urine. A first-voided morning specimen is preferred. Female patients should be instructed to clean external genitals before voiding, because the specimen should be free of vaginal discharge and feces. The specimen is sent to the laboratory or refrigerated if it must be kept longer than 1 hour. If left standing at room temperature for 5 hours, the specimen will not be suitable for culture; erythrocytes will decompose and casts will disintegrate. Nurses can obtain immediate information on ketones, pH, protein, glucose, and blood by using a Multistix reagent strip. The three principal constituents of urine are water, urea, and electrolytes, namely, sodium and chloride. In addition to many other substances found in the urine are all indications of possible disease. Routine urinalysis includes physical, chemical and microscopic examinations. Physical examination includes the following information: Volume. The amount of urine, both total daily volume and volume of each voiding, depends on a number of factors: fluid intake, fluid losses from other routes, fever, environmental temperature, age, ingestion of a high-protein diet (which produces more urine), or diuretic drugs. This indices is not significant because urinalysis is examination only one voiding. The amount per voiding normally depends on the person's bladder capacity. Color. Thecolorof normal urine depends on its concentration and varies from straw-yellow to the color of amber. The color of urine darkens on standing because of the oxidation of urobilinogen to urobilin. It begins in 30 minutes. When there is bleeding in the upper urinary tract, the urine may be dark red or smoky. Bleeding in the lower urinary tract produces red urine. Visible change of color due to presence of large quantity of erythrocytes is called - macrohematuria. Dark yellow urine may indicate the presence of urobilin or bilirubin. Milky white urine may be caused by pus or by fat globules released in the kidney as a result of nephrosis or severe trauma. Foods that may turn the urine red are rhubarb, beets, blackberries, and red food dyes. Bright yellow urine comes from ingesting large amounts of carotene (carrots or sweet potatoes). Many medications cause color changes in the urine. Table 4 lists some of these agents. Table 4. In average the specific gravity morning portion is varied from 1015-1025. Specific gravity is altered by severe kidney disease and by intravenous contrast media used during x-ray procedures.Specific gravity is increased by radiopaque contrast media, albumin, dextran, and in dehydration, chronic heart failure, and liver failure. Unusually high values for specific gravity, for example, above 1.030, suggests the presence of large amount of solid constituents in the urine, such as glucose in a diabetic patient. Low specific gravity indicates dilute urine and may occur with diabetes insipidus, acute tubular necrosis, released edema and alimentary dystrophia.
Chemical Analysis of Urine: Reaction of the Urine. The kidneys are important for maintaining acid-base equilibrium in the body. The kidneys are capable of removing the ions of hydrogen and hydrocarbonate from the blood and this is a mechanism by which pH of blood is maintained constant. Measure urine pH by using a dipstick, which is a multiple reagent strip treated with chemicals. Dip the dipstick into a fresh urine specimen and compare the color change with a standardized color on the bottle after waiting the specified amount of time.
URINALYSIS
Conclusion: presence of macrohematuria (red color and unaltered erythrocytes), much urates, cloudiness urine are typical for renal colic.
NECHIPORENKO'S METHOD is used to count erythrocytes, leucocytes and casts in 1 ml of urine for differential diagnosis between pyelonephritis and glomerulonephritis. The main advantage of this method is that an average sample of urine is taken for analysis and the presence of pus from the sex organs is excluded thus. In norm: erythrocytes count is to 1 x 106/L; leucocytes count is to 4 x 106/L; hyaline casts count is to 0,25 x 106/L. The amouth of leucocytes increases in pyelonephritis; the amount of erythrocytes and casts increases in glomerulonephritis.
Conclusion: increased leucocytes count indicates pyelonephritis.
ZIMNITSKY'S TESTS assess the concentration and excreted functions of the kidney by specific gravity and amount of the excreted urine. The main advantage of this method is that the renal function is tested without interfering with the normal life of the patient. The patient collects his urine at 3-hour intervals (8 portions during 24 hours). He begins to collect the urine from 9 o'clock in the morning and finishes at 6 o'clock in the morning the next day. Excreted Function. The volume of each portion of the urine determined. It is necessary to compare daily diuresis with amount of taken liquid. The normal daily amount of urine (daily diuresis) excreted by an adult varies from 1000 to 2000 ml. A normal individual should eliminate about 75-80% of the taken liquid during a day. The daily amount of urine below taken liquid is observed in patient with edema (negative diuresis). The amount of urine, both total daily volume and volume of each voiding, depends on a number of factors: fluid intake, fluid losses from other routes, fever, environmental temperature, age (a child excretes proportionately more than an adult), ingestion of a high-protein diet (which produces more urine), or diuretic drugs. The daily amount of urine over 2000 ml (polyuria) is observed in person who takes much liquid (physiologically or in diabetes mellitus), during resolution of edema and after taken diuretics, in early stage of chronic pyelonephritis, renal failure. The daily amount of urine below 500 ml (olyguria) may be of patient with kidney diseases (renal insufficiency) and unrenal diseases (vomitus, diarrhoea, limited intake of liquid, after hemorrhage, heart failure, pyrexia). The volumes of daily and night urine are compared and a conclusion is derived concerning daily (the first 4 portions) and nocturnal (the next 4 portions) diuresis. Normally the daily diuresis exceeds the nocturnal one in 2-3 times. Nocturnal diuresis (nocturia) prevails in renal insufficiency to indicate longer work of the kidneys because of their impaired functional capacity. Oliguria accompanied with nocturia is typical for heart failure. ZIMNITSKY'S TEST
Daily diuresis 300
Noctural diuresis 480 Round-the-clock diuresis 780 Taken liquid during day 1300 Conclusion: decreased amount of excreted urine (comparing with taken liquid) is typical for edema nocturia(prevalence of noctural diuresis), isuria (diviation between urine portions smaller than 100 ml), indicate disordered excretory function; deviation between specific gravity in urine portions smaller than 10 indicates disordered concentrative function. Such analysis can be in renal failure.
THE REHBERG'S TEST. To determine the functional renal condition it is possible to examine the glomerular filtration, the percentage of reabsorbed water. Renal insufficiency arises in cases where the mass of the active parenchyma is 20% and lower of normal weight. If a substance that is filtered in the glomeruli but is not reabsorbed or liberated in the tubules is used for the assessment of renal function, the clearance of this substance is actually equal to glomerular filtration. Using this phenomenon, Reberg proposed a test for studying the amount of filtration by endogenic or exogenic creatinine. If one assumes that creatinine content of plasma and glomerular filtrate is the same, it is possible to determine the degree of concentration of the glomerular filtrate as it passes the tubules. Blood is taken from the vein of the patient on a fasting stomach and creatinine concentration is determined. Urine is collected during 2 hours. Diuresis is measured thoroughly and creatinine content is determined. Next, using the formula of the amount of glomerular filtration and reabsorbtion percentage are calculated. EXAMINATION OF URINE. URINALYSIS (UA; routine UA) is an important routine screening test that gives information about the status of the renal and urinary tracts and the total body system. The test involves collection of a random sample of at least 100-200 ml of urine. A first-voided morning specimen is preferred. Female patients should be instructed to clean external genitals before voiding, because the specimen should be free of vaginal discharge and feces. The specimen is sent to the laboratory or refrigerated if it must be kept longer than 1 hour. If left standing at room temperature for 5 hours, the specimen will not be suitable for culture; erythrocytes will decompose and casts will disintegrate. Nurses can obtain immediate information on ketones, pH, protein, glucose, and blood by using a Multistix reagent strip. The three principal constituents of urine are water, urea, and electrolytes, namely, sodium and chloride. In addition to many other substances found in the urine are all indications of possible disease. Routine urinalysis includes physical, chemical and microscopic examinations. Physical examination includes the following information: Volume. The amount of urine, both total daily volume and volume of each voiding, depends on a number of factors: fluid intake, fluid losses from other routes, fever, environmental temperature, age, ingestion of a high-protein diet (which produces more urine), or diuretic drugs. This indices is not significant because urinalysis is examination only one voiding. The amount per voiding normally depends on the person's bladder capacity. Color. Thecolorof normal urine depends on its concentration and varies from straw-yellow to the color of amber. The color of urine darkens on standing because of the oxidation of urobilinogen to urobilin. It begins in 30 minutes. When there is bleeding in the upper urinary tract, the urine may be dark red or smoky. Bleeding in the lower urinary tract produces red urine. Visible change of color due to presence of large quantity of erythrocytes is called - macrohematuria. Dark yellow urine may indicate the presence of urobilin or bilirubin. Milky white urine may be caused by pus or by fat globules released in the kidney as a result of nephrosis or severe trauma. Foods that may turn the urine red are rhubarb, beets, blackberries, and red food dyes. Bright yellow urine comes from ingesting large amounts of carotene (carrots or sweet potatoes). Many medications cause color changes in the urine. Table 4 lists some of these agents. Table 4. Some Medications that Cause Changes in Urine Color.
Clarity (appearance). Urine is usually transparent when freshly voided. It turns cloudy on standing. Cloudiness in freshly voided urine becomes cloudy on standing. Cloudiness in freshly voided urine indicates bacteria, inflammation within the urinary tract, or the presence of sperm or prostatic fluid.
Odor. Normal, freshly voided urine is aromatic. Concentrated urine usually smells stronger than dilute urine. When urine stands, it may develop an ammonia smell due to bacterial action. Certain foods, such as asparagus, cause characteristic odor changes. Inflammatory reactions also alter the normal odor to ammonia smell (cystitis, pyelonephritis). Heavily infected urine has a particularly unpleasant fetid odor. A sweet (fruit) odor may indicate the presence of ketone bodies or acetone. It is found with diabetes mellitus, starvation, or dehydration. Other changes occur with medications, such as paraldehyde, vitamins, and antibiotics. Specific Gravity. The specific gravity of the urine varies from 1.001 to 1.040. Urinometer is used for measuring specific gravity. It gives information on the concentration of substances dissolved in it (urea, uric acid, salts) and characterizes the concentrating and diluting capacity of the kidneys. Specific gravity depends not only on the amount of particles dissolved but mainly on their molecular weight. Specific gravity of the morning portion is not important for diagnostics because it depends on many factors. If kidney function is normal, specific gravity indicates fluid status. High specific gravity in the absence of kidney failure usually indicates dehydration (after taken meat food, excessive perspiration), whereas low specific gravity under normal circumstances reflects overhydration (after vegetable meal, increased fluid intake, salt-restricted diet).
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Последнее изменение этой страницы: 2021-03-09; просмотров: 117; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 3.141.47.221 (0.024 с.) |