Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
Task 2. To investigate surface (skin) reflexes on stretch
1. Abdominal reflexes: a)superior – it’s caused by puncture irritation of abdomen skin in parallel of rib arc; the reflexes arc is closed at D6-D8 segments of spinal cord (from D – dorsal); b) intermediate – by similar irritation but at horizontal dimension at navel level; the reflexes arc is closed at D9-D10; c) inferior- in parallel to groin plica; the reflexes arc is closed at D11-D12. 2. Plantar reflex - is a plantar flexion of foot toes as a response of puncture irritation of external plantar limb; the reflexes arc is closed at L5-S2 and is in sciatic nerve. At injury of corresponding motor nerve and corresponding link of reflector arc the response reaction is decreased or disappeared (areflexy), muscular atony, atrophy are observed.
Fig. 21
Task 3. Deep (prophound) spinal reflexes investigation Biceps-reflex – is caused by irritation of muscle tendon above cubital joint by neurologic hammer. Answer reaction – hand flexion in cubital joint. The reflexes arc is closed at C5-C6. Afferent and efferent fibers are in muscular-cutaneous (skin) nerve structure. Triceps-reflex - is caused by hammer shock on triceps-muscle tendon, on 1-1,5 cm upper of posterior process of ulna. Answer reaction- muscular contraction and antebrachium (fore-arm) extension. The reflexes arc is closed at C6-C8. The fibers are in medianus, radialis and muscular-cutaneous nerves. Carpo-radialis reflex –is investigated by hummer shock onto awl-like processus of radius. Answer reaction – flexure in cubital joint and antebrachium pronation. Origin location: investigated person hand must be bended at obtuse angle in cubital joint; person’s examinated hand is supported by doctor’s hand at the locus between pronation and supination. The reflexes arc is closed at C5-C8. The fibers are in medianus, radialis and muscular-cutaneous nerves. Knee jerk or patellar tendon reflex - is caused by light shock of hummer on musculus quadriceps femoris tendon. Answer reaction – tibia extension. The reflexes arc is closed at L2-L4. Sensor and motor fibers are in femoral nerve. Every doctor must know how to elicit knee jerk. Knee jerk can be elicited by tapping the patellar tendon after the knee is semiflexed by placing one knee over the other while sitting on a chair or edge of a table. Immediately after the tendon tap the quadriceps femoris muscle contracts and there is jerking forward of the leg. There can be some alterations in knee jerk. Knee jerk is decreased or lost in: – Lesions in afferent neuron e.g. tabes dorsalis (Neurosyphilis). – Lesions in center, e.g. poliomyelitis. – Lesions in efferent neuron, e.g. lower neuron i.e. nerve pathway from anterior horn cell to muscle. – During sleep and anaesthesia. Knee jerk is increased or exaggerated in: – Upper motor neuron lesion. – Tetany, where there is increased neuromuscular excitability. – Neurotic subjects due to hyperexcitability of CNS. Pendular knee jerk occurs in lesion of neocerebellum which is characterized by hypotonia. In this type of knee jerk: – Contraction of quadriceps is weaker than in normal knee jerk. – Relaxation of quadriceps is quicker than normal knee jerk leading to quick fall of the leg like a dead weight. This is followed by vibrations or swinging of the leg like a pendulum. Hence the name pendular knee jerk. Hypotonia is the cause of the pendular knee jerk. Achilles’ reflex – the investigated person kneels on a chair for free feet hanging. To shock with hummer on achilles’ (calcaneus) tendon. Answer reaction – musculus gastrocnemius contraction and plantar foot flexion. The reflexory arc is closed at S1-S2. Sensor and motor fibers are in tibial nerve. If prophound myotatic reflexes are decreased or lost it testifies to reflector arc links disturbances. If answer reaction to the irritation is increased with significant excitement irradiation and involving other muscular groups into the answer reaction, reflector field spreading - it testifies to suprasegmentory central nervous system disorder existence.
5. Literature recommended: 1. Lecture course. 2. Mistchenko V.P., Tkachenko E.V. Methodical instructions for medical students (short lecture course).-Poltava, 2005.-P. 15-16. 3. Mistchenko V.P., Tkachenko E.V. Methodical instructions on Normal Physiology on practical classes for dental and medical students.-Poltava, 2005.-P. 36-40. 4. Ganong W.F. Review of Medical Physiology.-21st ed.-2003.-Section II. 5. Kapit W., Macey R.I., Meisami E. The Physiology Colouring Book: Harpers Collins Publishers, 1987.-P. 80. 6. Guyton – Ganong – Chatterjee. Concise Physiology /Ed. By Dr Raja Shahzad Gull: M.B.B.S., F.C.P.S., King Edward Medical College.-Lahore, 1998 (1st Edition).-P.295-301. 7. Guyton A.C. Textbook of Medical Physiology.-NY, 1992.-P.606-618.
1. Materials for self-control: A. Control questions: 1. Innervation segmentary character and its significance. 2. Spinal centers. 3. Spinal conductive tracts. 4. Spinal reflexes. 5. Spinal shock. LESSON 12 Topic studied actuality. Reception role sensations especially is rather essential: alive organism establishes organism connection with environment and orientation in it. Sensitivity disorders are also important in clinical neurological practice (together with motor function disturbances). We will illustrate a bit some clinical aspects and types of sensitivity disorders: Anesthesia – loosing one or another sensitivity type. There are several subtypes: – tactile; – pain or nociceptive (analgesia); – temperature (thermanesthesia); – localization sense loosing (topanesthesia); – stereognostic sense loosing (astereognosis); – joint-muscular sense loosing (batianesthesia); – general total anesthesia – all sensitivity types loosing. Hypoesthesia – sensitivity decreasing, sensations intensiveness reducing. It can touch both all sensitivity and its separate kinds. Hyperesthesia – increased sensitivity – occurs as a result of summation of irritation applied at investigation and irritation existing due to pathological process on the way of sensitive impulse. Dissociation - isolated disorder of one sensitivity types while normal other types at the same territory. Hyperpathy – sensation threshold increasing. Dysesthesia – touching is percepted like pain, warmth – like coldness and so on. Polyesthesia – human being tells about many sensations after just 1 stimulus action. Synesthesia – irritation feeling not only in the place of its making but in other region (from opposite side et al.). Thalamic syndrom - is a collection of symptoms resulting from damage of posterior-ventral portion of thalamus due to thrombosis. It has 3 main features: loss of almost all sensation from the opposite body side; ataxia; after a few weeks some sensory perception in the opposite side of body returns, but poorly. Herpes Zoster (Shingles). It is the infection of dorsal root ganglion. This causes severe pain in the dermatormal segment normally subserved by the ganglion, thus eliciting a segmental type of pain that circles halfway around the body. The disease is called herpes zoster, or “shingles” because of the eruption. The cause of the pain is presumably excitement of the neuronal cells of the dorsal root ganglion by the virus infection. Tic doulourex - lancinating pains occurs in some people over one side of the face in part of the sensory distribution area of the fifth or nineth nerve; this phenomenon is called tic douloureux (or trigeminal neuralgia or glosso-pharyngeal neuralgia). Allodyny – state at which pain is caused by non-harmful stimulation of normal skin (usual mechanic or thermal irritation causes pain).
Hyperalgesy – hypersensitivity to harmful stimuli. Hyperpathy – painful syndrome the distinguishing feature to which is enforced reaction with lacked beginning and afteraction which is remained after stimulation ending. 2. Study aims: To know: sensory information (noceoceptive, tactile, temperature and proprioceptive sensitivity) conduction ways; superficial and deep sensitivity physiological mechanisms. To be able to: to investigate pain, temperature, tactile, deep sensitivity; to draw superficial and deep sensitivity conductive ways. 3. Pre-auditory self-work materials. 3.1.Basic knowledge, skills, experiences, necessary for study the topic:
3.2. Topic content. Somato-sensor analizator – system providing organism connection with environment through skin and visible mucosae. It contains 3 types of receptors: – tactile (mechanoreceptors); – thermal (of warmth and coldness); – noceoceptive (of pain).
Tactile reception. Tactile reception is an important part of somato-sensor analizator. It is represented by touching and pressure receptors. These receptors are in strong functional interconnection with mechanoreceptors and proprioreceptors. They are located in skin different regions (maximal sensitivity is on fingers endings, foot). Touching sensation or pressure can be caused by indefinite points (tactile points). They are free nervous endings (Ruffini bodies, Pachini bodies et al.). Free nervous endings afferent fibers carry the information according to sensitivity type through spinal nerves, then through posterior columns fibers (Goll’s and Burdach’s fasciculi) to brain stem, thalamus and cortex (postcentral sulcus). Tactile sensitivity gives the imagination about subjects shape and their surface. Multiple, frequent irritation of them causes vibration sensation. Simultaneous several Pachini bodies involvement into reaction is the essential condition of vibration occurrence in skin. Skin superficial layers local anaesthesia doesn’t liquidate vibrational sensitivity and high-frequented receptors answer reactions. Temperature reception. Temperature analizator belongs to somato-sensor analizator too. Some sensor regions possess high sensitivity to temperature fluctuations. Temperature receptors are divided into receptors of warmth and of coldness. Coldness points amount is significantly predominant comparatively to warmth points. Their maximal accumulation is on face skin. Coldness receptors in human being are located in epidermis and directly under it and warmth receptors – primarily in derma (proper skin) superior and middle layer. Coldness receptors are connected with thin myelinized and warmth receptors – with non-myelinized fibers. Nociceptive sensation can occur either at injured stimulus action to special “noceoceptive” receptor – nociceptor, or at superstrong irritations of other receptors. Nociceptors are 25-40 per cent of all receptors. Nociceptors both of skin and of mucosa are represented by free non-incapsulated nervous endings of different shape (hairiness, spirals, plates et al.). Nervous fibers carrying impulses from these receptors reach spine posterior corns grey substance, where second neuron is originated from. Second neuron reaches brain columns white substance and further – thalamus from where it is projected widely into different cortical regions. Pain is defined as an unpleasant sensation and emotional experience associated with or without actual tissue damage. 2 main reasons: 1) tissues coverings injury; 2) oxygen respiration level changing: a) any substances disturbing oxidative processes in tissues plus b) blood supply stoppage ↓ pain ↓ sympathetic nervous system activation ↓ injured organ oxygen consumption inhibiting ↓ ↓ compensation of oxidative processes trophycs improvement insufficiency in it
tissular respiration coming to norm
Pain sensation has two components: 1) Fast pain 2) Slow pain. According to another classification, there are several pain components: 1) sensory – it is expressed in sensation; 2) affective – unpleasant emotions; 3) vegetative: – skin vessels dilation; – blood supply improvement leads to skin reddish; – skin vessels vasoconstriction; – circulation decreasing leads to skin palor; – hypotension; – tahysphygmy (frequent pulse); – midriasis (pupils dilation); – respiration rhythm changing; – at biliary colics – nausea, vomiting, hypotension, excessive sweat releasing; 4) motor: – reflex of avoiding or protection (for instance, at external injury); – muscular tension – at deep or visceral pain; 5) behavioral reactions; 6) consciousness; 6) memory; 8) motivations. Pain classification: a) acute or epicritic: – it is recognized rapidly; – it is determined easily; – adaptation is developed quickly to it;
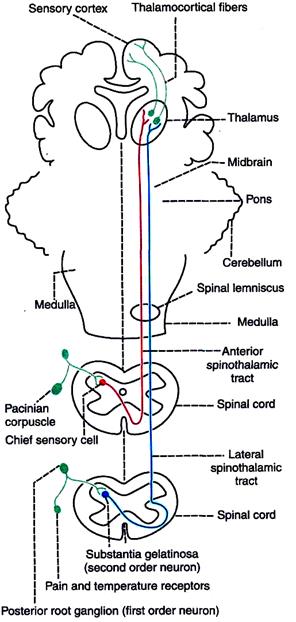
– it lasts not longer than stimulus action; – it is delt with nervous fibers of Aδ type (fast, conductance velocity is equal to 4-30 m/sec); b) chronic or protopathic: – it is recognized slowly; – it is localized badly; – it lasts for long time; – it is not accompanied by adaptation development; – it is more ancient than epicritic pain; – it is less perfect as a signal of danger; – it is linked with fibers of C type (speed is up to 3 m/sec). By occurrence place: 1) somatic: а) superficial (from skin): pinching, puncture; it is differentiated by appearance time: *early; *late; b) deep (from muscles, bones, joints, connective tissue): acute, subacute and chronic pain in joints; fits; headache; 2) visceral – from inner ogans: biliary colics, ulcer, appendicitis, spasms and others. Special forms: a) projected – state, at which the locus to which injuring stimulus acts to does not coincide to the place where one can feel the pain; b) neuralgia – subtype of projected pain when pain in the innervation region are observed at continuous irritations of nerve or posterior spine root; c) reflected – painful sensations caused by injuring irritations of inner organs are located not in a given organ but in separate surface locuses: - itch; - causalgias – burning stable continuous pain without definite reasons; d) central pain: - “painful anaesthesia” after posterior roots removal; - phanthomic pain – after amputations; - thalamic pain – at sensory ventral thalamic nuscle diseases; it is characterized by very big power. Whenever a pain stimulus is applied, first a bright, sharp and localized pain sensation is produced. This is called fast pain. It is followed by a dull, diffused and unpleasant pain. This is known as slow pain. The receptors for both components of pain are the same, i.e. free nerve endings. But afferent nerve fibers are different. The fast pain sensation is carried by A5 (g) fibers and the slow pain sensation is carried by С type of nerve fibers. Receptors of both components of pain are free nerve endings. Free nerve endings are distributed throughout the body. Scientists tell about 2 nociceptors types: mechanoreceptors -mechanic action leads to receptor membrane depolarization, permeability increasing for sodium ions in nervous fiber; then receptory potential and action potential (in nervous fiber) appear; chemonociceptors – react to the substances changing oxidative processes in tissues: – hydrochloric acid; – sulphuric acid; – acetic acid; – histamine; – acetylcholine; – hydrogen ions excess; – potassium ions excess; – somatostatin; – sunstance P; – prostaglandines E1, E2, F2α (aspirine, amidopyrine, analgine inhibit their formation). Nociceptors location: - skin; - muscles; - joints; - epiosteum; - subcutaneous cellulose; - inner organs; - vascular walls (big amount!). Conductive ways First order neurons are the cells in posterior nerve root ganglia. These neurons receive impulses of pain sensation from pain receptors through their dendrites and their axons reach the spinal cord. The fibers of fast pain sensation are carried by A5 afferent fibers. After reaching spinal cord, fibers synapse with marginal cells in posterior gray horn. Fibers transmitting impulses of slow pain belong to С type and these fibers synapse with substantia gelatinosa in the posterior gray horn. Second Order Neurons Marginal cells and cells of substantia gelatinosa form the second order neurons. Fibers from these cells ascend in the form of the lateral spinothalamic tract. Fibers of marginal cells for fast pain are long. Immediately after taking origin, the fibers cross midline via anterior gray commissure, reach anterolateral white column and ascend. These fibers form neo-spinothalamic tract—a part of lateral spinothalamic tract. These nerve fibers terminate in ventral posterolateral nucleus of thalamus. Some of fibers terminate in ascendng reticular system of brainstem. Fibers of slow pain which arise from substantia jelatinosa cross the midline and run along with fibers of fast pain as paleospinothalamic fibers in lateral spinothalamic tract. One fifth of these fibers terminate in posterolateral nucleus of thalamus. The remaining terminate in nuclei of reticular formation in brainstem in tectum of midbrain or in the gray matter surrounding deduct of Sylvius.
Third Order Neurons The third order neurons of pain pathway are the neurons of thalamic nucleus, reticular formation, tectum and gray matter around aqueduct of Sylvius. Axons from these neurons reach the sensory area of cerebral cortex. Some ones from reticular formation reach hypothalamus. Cente г s for Pain Sensation Cortical center for pain sensation is in the postcentral gyrus of parietal cortex. Fibers reaching hypothalamus are concerned with arousal mechanism due to pain stimulus. I PATHWAY OF PAIN SENSATION FROM VISCERA AND FACE The pain sensation from thoracic and abdominal viscera is transmitted by sympathetic (thoracolumbar) nerves. Pain from esophagus, trachea and pharynx is carried by vagus and glossopharyngeal nerves. Pain sensation from lace is carried by trigeminal nerve. II PATHWAY OF PAIN SENSATION FROM PELVIC REGION Pain sensation from deeper structures of pelvic region is conveyed by sacral parasympathetic nerves. Visceral pain Pain from viscera is unpleasant. It is poorly localized. CAUSES OF VISCERAL PAIN: 1. Ischemia: The substances released during ischemic reactions like bradykinin and proteolytic enzymes stimulate the pain receptors of viscera. 2. Chemical stimuli: The chemical substances like acidic gastric juice leaks from ruptured ulcers into peritoneal cavity and produce pain. 3. Spasm of hollow organs: Spastic contraction of muscles in gastrointestinal tract and other hollow organs of viscera cause pain by stimulating the free nerve endings. 4. Overdistention of hollow organs also causes pain. Referred pain The pain sensation produced in some parts of the body is felt in other structures away from the place of pain development. This is called referred pain. The deep pain and some visceral pain are referred to other areas. But, the superficial pain is not referred. EXAMPLES OF REFERRED PAIN 1. Cardiac pain is felt at the inner part of left arm and left shoulder 2. Pain in ovary is referred to umbilicus 3. Pain from testis is felt in abdomen 4. Pain in diaphragm is referred in right shoulder 5. Pain in gallbladder is referred to epigastric region 6. Renal pain is referred to loin. MECHANISM Dermatomal rule: Pain is referred to a structure, which is developed from the same dermatome from which the pain producing structure is developed. A dermatome includes all the structures or parts of the body, which are innervated by afferent nerve fibers of one dorsal root. For example, heart and inner aspect of left arm originate from the same dermatome. So, the pain in heart is referred to left arm. NEUROTRANSMITTER INVOLVED IN PAIN SENSATION Substance P is the neurotransmitter involved in pain sensation. It is secreted by the ending of pain nerve fibers in dorsal gray horn.
CONTROL OF PAIN SENSATION The central nervous system has its own control system, which inhibits the impulses of pain sensation. This is also called analgesia system. This control system is present in both brain and spinal cord. PAIN CONTROL SYSTEM IN BRAIN This actually blocks the pain impulses before entering the brain. This system is present in: 1) Gray matter surrounding aqueduct of Sylvius and 2) Raphe magnus nucleus in pons. The neurotransmitters involved in inhibition of pain by control system in brain are serotonin and opiate receptor substances namely endorphin, encephalin and dimorphic. PAIN CONTROL SYSTEM IN SPINAL CORD This is in posterior gray horn. The posterior gray horn is considered as the gateway for the pain impulses to reach the brain via spinothalamic tracts. Gate Control Theory The psychologist Ronald Melzack and the anatomist Patrick Wall Gate proposed the gate control theory for pain in 1965. They suggested that the gating system in the central nervous system opens and closes to allow the pain signals to the brain or to block the signals. According to them, the nerve fibers with smaller diameter carry pain stimuli through the gate mechanism present in spinal cord. But, the nerve fibers with larger diameter, which carry other stimuli such as touch, pass through the same gate. The larger nerves inhibit the transmission of pain signals by smaller nerves through the gate. When pain sensation is produced in any part of body, along with pain fibers, the other afferents particularly the touch fibers reaching the posterior column of spinal cord are also activated. The dorsal column fibers send collaterals to the cells of substantia gelatinosa in the posterior gray horn. Thus, some of the impulses ascending via dorsal column fibers pass through the collaterals and reach substantia gelatinosa. Here, the touch impulses inhibit release of substance P by the pain fibers ending on substantia gelatinosa. So the pain sensation is suppressed. Thus, the gating of pain in posterior gray horn level is similar to presynaptic inhibition. This forms the basis for relief of pain through rubbing, massage techniques and application of ice packs. The endogenous opioid peptides (pain relievers) released in response to pain stimulus also close the gate and block the pain signals. Acupuncture and electrical analgesia relieve pain by stimulating the release of endogenous pain relievers.
Melzack and Wall also suggested the role of brain in gate control. The sequence of events is as follows. The peripheral nerve fibers transmit the pain signals through open gates in spinal cord to thalamus. The signals are processed in thalamus and sent to sensory cortex. The perception of pain occurs in cortical level in context of the person's emotional status and previous experiences. The person responds to the pain based on the integration of all these information in the brain. Thus, the brain determines the severity and extent of pain. To minimize the severity and extent of pain, brain sends message back to spinal cord to close the gate. Now the pain stimulus is blocked and the person feels less pain. Brain sends the message to block the pain signals through opiate peptides and other natural pain relievers. If the brain sends message to open the gate wider, then the pain stimulus intensifies resulting in severe and prolonged pain. 3 variants of pain theory: 1) gates theory – see above; 2) theory of specificity: there are special receptors (nociceptors), special conductive ways and special zones in cortex. This theory is origined form R.Decart who wanted to answer the question how organism reactred to noceoceptive stimulus; 3) theory of pattern or intensiveness – excessive flow of impulses from different receptors (cutaneous, gustatory, sound and all) alongside without specific ways causes pain. ANTINOCICEPTIVE SYSTEM INCLUDES: 1) structures influencing on gelatinose substance (its activators): - cortex frontal lobe; - caudate nucleus (basal ganglion); - thalamus nucleus; - cerebellum neurons; - hypothalamic centers; - midbrain central grey near-aqueductal substance; - red nucleus; - black substance (midbrain); - reticular formation nuclei (several); 2) skin mechanoreceptors excitement leads to the fact that impulses part from them (on the way to medulla oblongata) come to gelatinose substance and activate it; 3) structures which synthesize row of substances: - endogenic opiates (dinorphine, endorphins, encephalines); - neurotensine (stronger than in opiates); - oxitocine (weakly); - vasopressine (weakly); - serotonin (in medulla oblongata) – strongly; - adrenaline (at stress, in sportsmen). Acupuncture causes activation of central grey near-aquedctal substance and, in turn: 1) activation of neurons of II-III gelatinose substance; 2) opioid peptides increasing in blood. TRACTS ANTERIOR SPINOTHALAMIC TRACT Anterior spinothalamic tract is formed by the fibers of second order neurons of the pathway for crude touch (Fig.21). Situation This tract is situated in anterior white funiculus near the periphery. Origin The fibers of anterior spinothalamic tract arise from the chief sensory cells of posterior gray horn which form the second order neurons of the crude touch pathway. The first order neurons are situated in the posterior nerve root ganglia. These neurons receive the impulses of crude touch sensation from the pressure receptors. The axons of these neurons reach the chief sensory cells. Course After taking origin, the fibers ascend in posterior gray horn for 2 or 3 segments in the same side. Then, the fibers cross obliquely in the anterior white commissure and enter the anterior white funiculus. Here, the fibers ascend through other segments of spinal cord, medulla, pons and midbrain and reach thalamus. When the tract ascends through brainstem, the number of fibers is considerably reduced as some of the fibers form the collaterals and reach the reticular formation of brainstem. Termination The fibers of anterior spinothalamic tract terminate in the ventral posterolateral nucleus of thalamus. The cells of this thalamic nucleus form the third order neurons of the pathway. The fibers from thalamic nucleus carry the impulses to some sensory areas of cerebral cortex. Function This tract carries impulses of crude tactile (protopathic) sensation. The bilateral lesion of this tract leads to loss of crude touch sensation and loss of sensations like itching and tickling. The unilateral lesion of this tract causes loss of crude touch sensation in the opposite side below the level of lesion.
Fig.2 2. Spinothalamic tracts and pathways for crude touch, pain and temperature sensations. Anterior spinothalamic tract carries crude touch sensation. Lateral spinothalamic tract carries pain and temperature sensations. LATERAL SPINOTHALAMIC TRACT Lateral spinothalamic tract is formed by the fibers from the second order neurons of the pathway for the sensations of pain and temperature (Fig.20.). Situation This tract is situated in the lateral funiculus towards medial side, i.e. near the gray matter. Origin The fibers of lateral spinothalamic tract take origin from substantia gelatinosa of Rolando situated in the posterior gray column. The first order neurons are in posterior nerve root ganglia. Course Axons from second order neurons mostly cross to the opposite side and reach the lateral column of same segment. Few fibers may ascend one or two segments, then cross to the opposite side, and ascend in the lateral column. All the fibers pass through medulla, pons and midbrain towards thalamus along with the fibers of anterior spinothalamic tract. The fibers of lateral spinothalamic tract form spinal lemniscus along with the fibers of anterior spinothalamic tract at the lower part of medulla. Some of the fibers of lateral spinothalamic tract form collaterals and reach the reticular formation of brainstem. Termination The fibers of lateral spinothalamic tract terminate in the ventral posterolateral nucleus of thalamus. From here, third order neuron fibers relay to the somesthetic area of cerebral cortex. Function The fibers of this tract carry impulses of pain and thermal sensations. The unilateral lesion or sectioning of the lateral spinothalamic tract causes loss of pain (analgesia) and temperature (thermoanesthesia) below the level of lesion in the opposite side. The bilateral section of this tract leads to loss of pain and temperature sensations on both the sides below the level of lesion.
FASCICULUS GRACILIS (TRACT OF GOLL) AND FASCICULUS CUNEATUS (TRACT OF BURDACH) The ascending tracts in the posterior white funiculus of the spinal cord are formed by the fibers from posterior root ganglia. Thus, both the tracts are constituted by the fibers of first order neurons of the sensory pathway. The fibers are uncrossed fibers. Situation These two tracts are situated in posterior white funiculus of spinal cord. In the cervical and upper thoracic segments of spinal cord, the posterior white funiculus is divided by posterior intermediate septum into medial fasciculus gracilis and lateral fasciculus cuneatus. Thus, the fasciculus gracilis is situated between posterior median sulcus and posterior median septum on one side and the posterior intermediate sulcus and posterior intermediate septum on the other side. The fasciculus cuneatus is bound medially by posterior intermediate septum and sulcus and laterally by posterior gray horn, tract of Lissauer and posterior nerve root. Origin Fibers of these two tracts are the axons of I order neurons. The cell body of these neurons is in the posterior root ganglia and the fibers form the medial division (bundle) of the posterior nerve root. After entering the spinal cord, the fibers ascend through the posterior white funiculus. These fibers do not synapse in the spinal cord. Some of the fibers of medial division of posterior nerve root descend through the posterior white funiculus in the form of fasciculus interfascicularis or comma tract of Schultze. Course The fasciculus gracilis contains the fibers from the lower extremities and lower parts of the body, i.e. from sacral, lumbar and lower thoracic ganglia of posterior nerve root. Fasciculus cuneatus contains fibers from upper part of the body, i.e. from upper thoracic and cervical ganglia of posterior nerve root. Termination These two tracts terminate in the medulla oblongata. The fibers of fasciculus gracilis terminate in the nucleus gracilis and the fibers of fasciculus cuneatus terminate in the nucleus cuneatus. The cells of these medullary nuclei form the second order neurons. The axons of the second order neurons form the internal arcuate fibers. The internal arcuate fibers from both the sides cross the midline forming sensory decussation and then ascend through pons and midbrain as medial lemniscus. The fibers of medial lemniscus terminate in ventral posterolateral nucleus of thalamus. From here, fibers of the third order neurons relay to cerebral cortex. Functions The tracts of the posterior white funiculus convey impulses of following sensations: 1. Fine, i.e. epicretic tactile sensation. 2. Tactile localization: It is the ability to locate the area of skin where the tactile stimulus is applied. 3. Tactile discrimination: It is the ability to recognize the two stimuli, which are applied over the skin simultaneously. 4. Sensation of vibration: This is the ability to perceive the vibrations (from a vibrating tuning fork placed over bony prominence) conducted to deep tissues through skin. 5. Conscious kinesthetic sensation: It is the sensation (awareness) of various muscular activities in different parts of the body. 6. Stereognosis: It is the ability to recognize the known objects by touch with closed eyes. The lesion in the fibers of these tracts or lesion in the posterior white column leads to the following symptoms. The symptoms appear on the same side below the lesion. 1. Loss of fine tactile sensation. However, crude touch sensation is normal. 2. Loss of tactile localization. 3. Loss of two point discrimination. 4. Loss of sensation of vibration. 5. Astereognosis: It is the inability to recognize known objects with closed eyes. 6. Lack of ability to differentiate the weight of different objects. 7. Loss of proprioception: There is inability to appreciate the position and movement of different parts of the body. Because of the loss of proprioception, the voluntary movements become incoordinated, slow and clumsy. This condition is known as sensory ataxia or posterior column ataxia.
|
||||||||||||||||||||||||
|
Последнее изменение этой страницы: 2021-03-09; просмотров: 133; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 18.219.236.62 (0.24 с.) |

 ↓
↓