Заглавная страница Избранные статьи Случайная статья Познавательные статьи Новые добавления Обратная связь КАТЕГОРИИ: ТОП 10 на сайте Приготовление дезинфицирующих растворов различной концентрацииТехника нижней прямой подачи мяча. Франко-прусская война (причины и последствия) Организация работы процедурного кабинета Смысловое и механическое запоминание, их место и роль в усвоении знаний Коммуникативные барьеры и пути их преодоления Обработка изделий медицинского назначения многократного применения Образцы текста публицистического стиля Четыре типа изменения баланса Задачи с ответами для Всероссийской олимпиады по праву 
Мы поможем в написании ваших работ! ЗНАЕТЕ ЛИ ВЫ?
Влияние общества на человека
Приготовление дезинфицирующих растворов различной концентрации Практические работы по географии для 6 класса Организация работы процедурного кабинета Изменения в неживой природе осенью Уборка процедурного кабинета Сольфеджио. Все правила по сольфеджио Балочные системы. Определение реакций опор и моментов защемления |
Classification of Chronic Obstructive Pulmonary Disease by Severity
FEV1 - forced expiratory volume in 1 second; FVC - forced vital capacity. Clinical features Patients who have smoked > 20 cigarettes per day for > 20 yr may develop a productive cough in their 40s or early 50s. Exertional dyspnea usually does not become severe enough to warrant a visit to a physician until COPD patients are in their 50s lo mid-60s. Sputum production is insidious in onset, initially occurring only in the morning. Daily volume rarely exceeds 60 mL. Sputum is usually mucoid but becomes purulent during an exacerbation. Acute chest illnesses-characterized by increased cough, purulent sputum, wheezing, dyspnea, and occasionally fever-may occur from time to time. (A history of wheezing and dyspnea may lead to the erroneous diagnosis of asthma.) As COPD progresses, the intervals between acute exacerbations tend to become shorter. Late in the disease, an exacerbation may cause severe hypoxemia with cyanosis, which is accentuated if erythrocytosis is present. Morning headache may indicate hypercapnia. Hypercapnia with more severe hypoxemia, sometimes with erythrocytosis, is common in end-stage disease. Weight loss occurs in some patients. Objective examination. Early in COPD, physical examination of the chest may not be remarkable except for auscultation of expiratory wheezes. As airway obstruction progresses, hyperinflation of the lungs becomes evident. The anteroposterior diameter of the chest in creases because the lungs are near full inspiration and because emphysema increases total lung capacity. The diaphragm is depressed, and its motion limited. Breath sounds are decreased, and heart sounds become distant. Signs of pulmonary hypertension and right ventricular hypertrophy are usually not detectable because emphysematous lung tissue is interposed between the heart and anterior chest wall. A few coarse crackles are often heard at the lung bases. An enlarged, tender liver indicates heart failure. Neck vein distention, especially during expiration, may occur in the absence of heart failure because of increased intrathoracic pressure. Asterixis may accompany severe hypercapnia. The patient with end-stage COPD is often a dramatic sight - standing before a counter leaning forward with arms outstretched and weight supported on the palms. The accessory respiratory muscles of the neck and shoulder girdle are in full use. Expiration often occurs through pursed lips. The chest appears overinflated, often with paradoxic in drawing of the lower interspaces. Cyanosis may be present. Additional methods of examination Clinical blood analysis: without significant changes, sometimes secondary erythrocytosis; in progression assess leukocytosis, neutrophilia, accelerated ESR. Sputum analysis: sputum in patients with stable chronic bronchitis is mucoid. During an exacerbation, sputum usually becomes purulent, with an influx of neutrophils. X-ray examination: in severe disease, persistent, marked overdistention of the lungs is indicated in the frontal view by a low, flat diaphragm and in.the lateral view by widening of t he retrosternal airspace and an increase in the angle formed by the sternum and diaphragm from acute to ≥ 90°. The heart shadow tends to be long and narrow. Test of ventilatory function (spirometric recording and pneumotachymetry): pulmonary function tests are helpful in diagnosing COPD, in assessing its severity, and in following its progress. Forced expiratory spirometry quantifies airway obstruction. Airflow obstruction is an important indicator of symptomatic respiratory insufficiency and of the likelihood of blood gas abnormalities. The FEV1 and the FEV1/FVC fall progressively as the severity of COPD increases. The FEV1 is less variable than other measurements of airway dynamics and can be predicted more accurately from age, sex, and height. Functional residual capacity and residual volume are increased; vital capacity is decreased. Roughly comparable information can be obtained from the forced expiratory flow-volume loop.
ECG: diagnosing pulmonary hypertension and cor pulmonale in COPD is difficult without right-sided heart catheterization. On the ECG, an R or R' wave as large as or larger than the S wave in lead V1 and R wave smaller than the S wave in lead V6 and right-axis deviation >110° without right bundle branch block support the diagnosis of cor pulmonale. Echocardiography: especially with an esophageal transducer, and pulsed Doppler techniques to estimate mean pulmonary arterial pressure can be used to assess pulmonary hypertension and right ventricular function. Left ventricular size and performance are generally normal inpatients with COPD and no other associated cardiac abnormalities. The right ventricular ejection fraction is frequently abnormal, especially during exercise. Blood gas analysis: arterial blood gas measurements detect hypoxemia and hypercapnia and determine their severity. In the early stages of COPD, measuring arterial blood gases reveals mild or moderate hypoxemia without hypercapnia. As the disease progresses, hypoxemia becomes more severe and hypercapnia supervenes. Hypercapnia occurs with increasing frequency as the FEV1 falls below 1L. Blood gas abnormalities worsen during acute exacerbations and may worsen during exercise and sleep.. CHRONIC BRONCHITIS Chronic bronchitis is chronic inflammation of the bronchi and bronchioles. Etiology - smoking, pollution of the environment by products of incomplete fuel substances combustion, organic and inorganic dust; - infection (bacterial, viral, micoplasms, fungus); - congenital occurrences in lesser circulation on heart failure; - exposure of metabolic products on renal failure; - result of acute bronchitis. Classification of chronic bronchitis (by N.R Paleev, 1990) I. According to the character of inflammatory process: - simple (catarrhally); - purulent; - muco-purulent; - special forms: hemorrhagic and fibrinous. //. According to the presence of bronchial obstruction: - obstructive bronchitis (stages: I, II, III; duration: simple, moderate grave, grave); - non obstructive bronchitis. III. According to the level of bronchi injury: - proximal; - distal; - diffuse. IV. According to the duration: - latently; - with infrequent aggravations; - with frequent aggravations; - continuously progress. V. According to the phases: - progress; - remission. VI. According to the complications: - emphysema of the lungs; - hemoptysis; - pneumonia; - respiratory failure; - "Cor pulmonale". Pathogenesis. On chronic bronchitis occurs development of classic pathogenetic triad: - hypercrinia (mucous hyperproduction); - dyscrinia (increased sputum viscosity); - mucostasis (overcrowding of the sputum in bronchi). Approaching to the bronchi of infection agent leads to the sensebilization and autosensebilization of the organism. There are the next mechanisms of the bronchial obstruction development: - brochospasm; - inflammatory edema and bronchial wall infiltration; - hyper- and dyscrinia; - hypotonic dyskinesia of large bronchi;
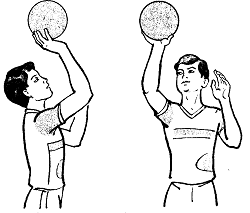
- collapse of small bronchi during expiration; - mucus lays hyperplasic reaction. Clinical features The main complaints in patients with chronic bronchitis are moist cough, general weakness, perspiration and dyspnea in cause of bronchium obstruction. Cough is commonly periodic, moist with difficult sputum expectoration. Sputum expectoration is the most important symptom of chronic bronchitis. On early stages of the disease the sputum may be mucous, tenacious consistency, glass-like, for the period of progression becomes mucopurulant or purulent. The 24-hours amount of sputum is usually 50-70 ml, due to development of bronchiectasis significantly increase to 100-200 ml. Dyspnea - commonly has expiratory character and its appearing indicates presence of bronchial obstruction and emphysema. Objective examination. General patient's condition is usually satisfactory. On progression and complications advance general patient's condition may be from middle grave to grave. Due to gradual chronic hypoxia and intoxication possibly will be observed perspiration and subfebrile or febrile temperature. The posture of the patients is frequently active. On progression and complications advance is forced in form of orthopnea - sitting position fixing the shoulder girdle in order to reduce dyspnea via assists the accessory muscles and diaphragm to take part in respiration. The color of the skin and visible mucous depends on the stage and variant of obstruction. In initial stage the color of the skin and visible mucous is without any particularities. Due to the chronic bronchitis progression observe diffuse cyanosis with peripheral edema via to the "cor pulmonale" development. In obstructive emphysema bronchi spasm occurs during expiration therefore alveolar air is a little change and in spite for constant dyspnea the skin and visible mucous cyanosis isn't specific. In purulent chronic bronchitis detect the form of the Hippocratic nails. The data of chest inspection, palpation and percussion include clinical features of bronchium obstruction: emphysematous form of the chest with accessory respiratory muscles participation in the breathing act, decreased excursion of the chest, badly transmitted vocal fremitus and generalized bandbox sound over the lungs during percussion. Auscultation of the lungs. Auscultative data in patients with chronic bronchitis is characterized by sibilant and sonorous dry rales of different tone and intensity over the pathologically increased vesicular breathing. In localized affection of medium and large bronchi insignificant amount of low pitched and soft rales are heard. Accumulation of the viscous secret in bronchi via active inflammation, are accompanied by coarse and medium bubbling rales that can be altered by coughing or deep inspiration.
|
||||||||||||||||
|
Последнее изменение этой страницы: 2016-08-26; просмотров: 471; Нарушение авторского права страницы; Мы поможем в написании вашей работы! infopedia.su Все материалы представленные на сайте исключительно с целью ознакомления читателями и не преследуют коммерческих целей или нарушение авторских прав. Обратная связь - 3.141.244.201 (0.014 с.) |